
1.3M
Downloads
272
Episodes
A UK based Emergency Medicine podcast for anyone who works in emergency care. The St Emlyn ’s team are all passionate educators and clinicians who strive to bring you the best evidence based education. Our four pillars of learning are evidence-based medicine, clinical excellence, personal development and the philosophical overview of emergency care. We have a strong academic faculty and reputation for high quality education presented through multimedia platforms and articles. St Emlyn’s is a name given to a fictionalised emergency care system. This online clinical space is designed to allow clinical care to be discussed without compromising the safety or confidentiality of patients or clinicians.
Episodes

Monday Jun 19, 2023
Ep 220 - Penetrating Injuries with John O’Neil at the PREMIER Conference
Monday Jun 19, 2023
Monday Jun 19, 2023
This episode of the podcast is a live recording from the PREMIER Conference of John O Neil discussing penetrating injuries with learning points that are useful for clinicians who look after both adult and paediatric patients.
There are three main mechanisms – violence, impalement and self harm, although the first is by far the most common.
Penetrating injuries are rare but have significant morbidity and mortality. The key is early and accurate diagnosis, and many can be managed conservatively. The distribution of penetrating injuries across the UK differs widely, with most in the London area, although as seen in the news recently can happen anywhere.
Remember how traumatic it is to be a trauma patient. We put you on a bed, cut off your clothes, stick needles in you and take your family away. Some will also just not engage with you (teenage boys particularly) making assessment difficult. Be kind. Don’t get frustrated.
Physiologically there may be a strong vagal response that can hide some of the signs we’d expect. Also, bear in mind the events prior to the injury – the child may have been running a considerable distance (before and after the incident) raising their lactate (but don’t assume this is the cause). Children tend to ‘fall off a cliff’ – they appear well, but can suddenly decompensate – keep the momentum to definitive management going and do not be falsely reassured.
John mentioned a great friend of St Emlyn’s Vic Brazil and we would heartily endorse you have a look at her work.
You can find more information about the Reducing Knife Crime initiative here

Saturday Jun 17, 2023
Ep 219 - Blast Injuries with Chris Hillman at the PREMIER Conference
Saturday Jun 17, 2023
Saturday Jun 17, 2023
Chris brought us his reflections amnd knowledge from some of his extensive experience as a military EM consultant in two wars. Blast injury could be blunt, penetrating, may involve major haemorrhage: you have to expect any injury possible. It’s worldwide and it’s getting more common.
Blast injury affects every body cavity, but it is the CABC approach that matters, Doing the basics well is still the key. Bleeding points may not be obvious so apply tourniquets wherever stops the bleeding.
Often patients will not arrive in ones or twos but as a whole group affected by an incident, so it is vital we are prepared. The Paediatric Blast Injury Field Manual is a free resource available to download here and is highly recommended.
Chris Hillman is a Consultant in Emergency Medicine and Paediatric Emergency Medicine, working in Southampton. Serving in the Royal Navy since university, he has deployed on Ships, Submarines and with Commando units globally, and with the Army to Afghanistan and Iraq. He is the outgoing Consultant Advisor in Emergency Medicine and Clinical Director Commando Forward Surgical Group.

Thursday Jun 15, 2023
Ep 218 - Non epileptiform seziures with Steve Warriner at the PREMIER Conference
Thursday Jun 15, 2023
Thursday Jun 15, 2023
This is the second in our series of talks recorded live in June 2023 at the PREMIER conference.
Looking after patients with non-epileptiform seizures are a challenging, and common, event in the Emergency Department. 10% of attendances at paediatric neurology clinics are thought to be 'functional' and a lot of these will also present to the ED. These problems can involve a wide range of physical or sensory manifestations, almost all of wide have significant differentials which we cannot miss.
A large number of these patients can end up with an incorrect diagnosis, some of this due to confirmation bias by clinicians, but also some with psychogenic non-epileptiform seizures may coexist with organic problems.
The history is key and can be helped significantly by watching videos of events. There may be other factors giving a clue to a non-epileptic cause. Sometimes this will only happen in one place, like school, and the history may be inconsistent. Awareness and generalised bilateral movements, with episodes that are different each time all point to a non epileptiform origin. And then there are symptoms just 'not fitting' with our knowledge of dermatomal distribution.
There are Red Flags - Events happening during exercise, neurological signs, unpredictability and patterns to the events all point to a more sinister diagnosis
Management is incredibly difficult, particularly in trhe ED. Don't suggest an organic diagnosis and leave some ambiguity. There is time to get more information and there are few definitive diagnostic tests. EEGs are notoriously unreliable. Self help groups can help.
Steve Warriner has worked as a paediatrician at the QA in Portsmouth for the last 16 years. He trained in various regions in the UK including the Midlands, Yorkshire and the North East of England before working in Somerset for a brief period. He has a particular interest in epilepsy and neurological conditions in children and lead the district epilepsy service in Portsmouth. He teaches on the British Paediatric Neurology Association epilepsy training courses both in the UK and across the world. He was part of the team who designed and implemented the training course (initially in Myanmar) and the method of cascade training has recently been recognised by the World Health Organisation and the course now runs in nearly 30 counties in 3 languages. Steve recently chaired a multidisciplinary working group to update the Advanced Life Support Group guideline for management of prolonged seizures. In his spare time, Steve is a triathlete who qualified for and competed in the World Ironman Championship race in Hawaii in 2022.

Tuesday Jun 13, 2023
Ep 217 - Weaning the wheezy child with David James at the PREMIER Conference
Tuesday Jun 13, 2023
Tuesday Jun 13, 2023
This is the first in a series of podcasts, recorded live at the Premier Conference in Winchester.
In this episode, David James challenges our current practice when we give a 'weaning plan' for children discharged with wheeze.
There is a plan here that you can review and give to patients and their carers.
More information at these excellent websites
David James has been a PEM Consultant at University Hospital Southampton since 2018. His main interests are in training and education, adolescent emergency medicine and Quality Improvement. He is the Divisional Director of Medical Education and a Training advisor on the PEMISAC. He is the acute care lead for Wessex Healthier Together and has led several projects including those around acute wheeze at UHS and regionally. Outside of work he enjoys swimming, cycling and running and is extremely average at triathlons.

Saturday Jun 10, 2023
Ep 216 - April 2023 Monthly Round Up: HALO procedures and Blood Transfusion
Saturday Jun 10, 2023
Saturday Jun 10, 2023
The monthly round up of all the blog posts at St Emlyn's, including a deep dive into HALO (high acuity, low occurrence) procedures and blood transfusion.
Thanks again for listening. Please do like and subscribe here.

Wednesday May 03, 2023
Ep 215 - March 2023 Monthly Round Up
Wednesday May 03, 2023
Wednesday May 03, 2023
Our monthly podcast round up from St Emlyn's Blog. This month Simon and Iain discuss the prehospital use of troponin measurement in the assessment of patients with chest pain and the use of AI in medicine, as well as an update about St Emlyn's WILD.
Please do like and subscribe

Monday Apr 24, 2023
Ep 214 - Shock from St Emlyn’s Medical School
Monday Apr 24, 2023
Monday Apr 24, 2023
This is the first podcast in our new series from St Emlyn's Medical School. They are specifically aimed at healthcare students and focus on the Medical Licensing Assessment (UK) presentations in particular but will be useful wherever you listen in the world.
Each episode has a standard format with a case to set the scene, a set of learning objectives, a discussion, a summary and a case resolution.
There are comprehensive listening notes on the dedicated website, as well as a growing set of other resources.
We hope you enjoy listening. The rest of the podcasts can be found on Spotify, or wherever you get your podcasts.
The music for this series (just as it is for the St Emlyn's Podcast) is composed by Greg Beardsell

Monday Apr 17, 2023
Ep 213 - Sensitivity and Specificity (CAN 10)
Monday Apr 17, 2023
Monday Apr 17, 2023
The latest CAN is one of our brand-new 'revision editions' -- brief podcasts aimed at covering the essentials of critical appraisal for medical students and junior doctors preparing for exams.
With the help of Gregory Yates, an academic doctor based in Manchester, this episode introduces two core concepts: sensitivity and specificity. These are two ways of thinking about the accuracy of a diagnostic test. Knowing the sensitivity and specificity of an investigation will give you a decent idea of how it should be used in the emergency department.
Sensitivity (Sn) describes the chance that a test will be positive if your patient has the condition you're testing for. Some people call it the 'true positive rate' or alternatively the positivity in disease (PID) rate. If you need a hand remembering it, you can always remember that PID is a sensitive issue.
Meanwhile, specificity (Sp) considers the chance of a test being negative if the patient doesn't have the condition you're testing for. It's the 'true negative rate' or alternatively the negativity in health (NIH) rate. There are times when we particularly need a test to have a high sensitivity. This is generally when we want to be particularly confident that a test accurately identifies everyone with the relevant condition because we really don't want to miss it. We need a high sensitivity to rule out disease. (Sn-uff it out). At other times, we need to be confident that a patient with a positive test actually has the disease - for example, if the treatment is unpleasant or involves exposing patients to risk. In that case, we want a high specificity to rule in disease. (Sp-in it in).
In this CAN, we use D-Dimer as an example of a very sensitive investigation: it’s positive in nearly 100% of cases of venous thromboembolism. Specificity describes the likelihood that the test will be negative if your patient does not have the disease. We use HbA1c as an example of a highly specific investigation: it’s rarely used in the emergency department, but if it’s elevated, we can be almost certain that the patient is diabetic. HbA1c is almost never (<1%) raised in non-diabetics.
The trouble is, many patients with a positive D-Dimer do not have a venous clot, and the majority of diabetics will have a normal HbA1c! No test is perfect, and we discuss how emergency physicians weigh up sensitivity and specificity when choosing which investigations are the best "fit" for clinical decision-making. By the end of this CAN, you will be ready to do the same -- in your exams, and on the shop floor.

Monday Mar 20, 2023
Ep 212 - February 2023 Monthly Round Up
Monday Mar 20, 2023
Monday Mar 20, 2023
Our regular monthly round up and chat from the St Emlyn's blog. We talk about the use of artificial intelligence in research and the use of remifentanil instead of neuromuscular blockade in rapid sequence intubation. Plus more about the StEmlynsWILD conference and Simon's new role as Dean of RCEM and how you can get involved.

Monday Feb 27, 2023
Ep 211 - Semi structured interviews (CAN 9)
Monday Feb 27, 2023
Monday Feb 27, 2023
Long term listeners to the St Emlyn’s podcast may remember our series entitled ‘Critical Appraisal Nuggets’ (CANs). We are absolutely delighted to reinvigorate this project under the leadership of Professor Rick Body, with the episode on semi structured interviews.
In this easily digestible and succinct podcast Rick and Laura Howard go through the pros and cons of setting up semi structured interviews and how these can be used effectively in qualitative research.
In the latest episode, we cover a qualitative research technique: semi-structured interviews. Qualitative research might be out of your comfort zone: we’re generally more comfortable with quantitative measures – numbers and statistics. It’s something they have experience with, having previously published a paper exploring the impact of events that happen at work on the wellbeing of emergency physicians. This was a labour of love for Laura. Laura wrote a powerful blog about it here.
Semi-structured interviews are a great way to get the really rich data we need to understand something in greater depth. They allow us to ask ‘why?’ as well as just ‘what?’, ‘who?’ and ‘when?’. But reading qualitative research papers can be difficult when it takes us out of our comfort zone. In this CAN podcast, Laura and Rick take us through what semi-structured interviews are, why we might use them, how you design and conduct them, and they also have some pearls of wisdom about how to make transcribing them a lot less painful. By the end, we hope that you’ll feel confident with the basics of the technique. And if you want to practice your critical appraisal, why not put their study under the microscope?

Monday Feb 13, 2023
Ep 210 - January 2023 Monthly Round Up
Monday Feb 13, 2023
Monday Feb 13, 2023
Lots of chat about St Emlyn's WILD and just what you can expect if you join us in the Lake District in June, as well as discussion about ECMO in cardiac arrest and just how many of our patients with 'minor head injuries' will actually have ongoing symptoms weeks and even months later.
Click here to buy tickets for #StEmlynsWILD

Monday Jan 16, 2023
Ep 209 - November and December 2022 Round Up
Monday Jan 16, 2023
Monday Jan 16, 2023
A special double edition covering the blog posts from November and December and more. We discuss evidence based medicine with the DoseVF trial, and more from RECOVERY, discussion about 'what is downtime' and how we organise follow up for patients who don't live in our area and what happened at the amazing London Trauma Conference
We also announced some of the plans for StEmlynsWILD. Look out for booking details and more in the coming weeks.

Saturday Dec 10, 2022
Ep 208 - What is Wellbeing with Liz Crowe
Saturday Dec 10, 2022
Saturday Dec 10, 2022
Wellbeing is very complex, as it is an individual construct that is strongly aligned and interpreted through a lens of personal values, philosophy, culture, faith, and goals for life. Most importantly, wellbeing is dynamic rather than homeostatic and a subjective state determined by the individual.
Yet we use the term wellbeing to describe a wide variety of different things (often in terms of being the opposite of burnout which it most certainly isn't).
In this second episode of our series Liz Crowe discusses in detail what the literature says about wellbeing and how we may be able to use this going forward.
Please do like and subscribe. Thanks for listening.
Sunday Nov 27, 2022
Ep 207 - Burnout with Liz Crowe
Sunday Nov 27, 2022
Sunday Nov 27, 2022
Burnout is a term that seems to be used a lot these days, but what does it really mean? In this episode Dr Liz Crowe explains all, and will almost certainly change the way you view burnout.
Liz, who be well known to St Emyn's audiences, has just completed her PhD on "Understanding the risk and protective factors for burnout and wellbeing of staff working in the Paediatric Intensive Care Unit: PICU staff wellbeing" and has an unrivalled real world and evidence based experience of what these terms really mean.
In this first in a special series Liz goes into depth describing not only what burnout is, but how it can be measured (and the limitations of this) and most importantly how this is a system issue and not a diagnosis.
In the next episode we will discuss another commonly used term 'wellbeing'.
We think this series is incredibly important and hope you will help us share it far and wide. You can read the accompanying blogpost here.

Monday Nov 14, 2022
Ep 206 - October 2022 Round Up
Monday Nov 14, 2022
Monday Nov 14, 2022
In our new regular slot of the middle Monday of the month we're delighted to bring you the highlights from the St Emlyn's blog this month.,
Iain and Simon chat about batching in EDs, Ossilation in decision making and a whole lot more about trauma (chest drains, extrication, sex and TXA and rib fixation).
Please do like and subscribe and keep an eye out for our new sister website St Emlyn's Medical School and it's podcast series coming soon.

Tuesday Oct 18, 2022
Ep 205 - September 2022 Round Up
Tuesday Oct 18, 2022
Tuesday Oct 18, 2022
Join Iain and Simon for this month's round up of September's blog content from St Emlyn's. They discuss managing harm in the ED; management of traumatic brain injury; Head Up mechanical CPR and fentanyl in RSI.
Lots to think about and discuss. Please do like and subscribe and get in touch if there is anything you'd like us to cover on the blog and podcast, or perhaps you'd even like to write something for publication.

Saturday Oct 08, 2022
Ep 204 - August 2022 Round Up
Saturday Oct 08, 2022
Saturday Oct 08, 2022
This is our round up of all that happened on the St Emlyn's blog in August 2022 (yes - we know it's a bit late, but there's been a lot going on!).
Listen to Simon and Iain discuss the latest therapies in COVID, particularly Baricitinib, calcium in trauma and how we find balance in our work-life blend.
Please do like and subscribe to the podcast and tell your friends and colleagues. We've lots of exciting stuff coming your way over the next few months.

Sunday Aug 07, 2022
Ep 203 - June and July 2022 Round Up
Sunday Aug 07, 2022
Sunday Aug 07, 2022
Simon and Iain run through the latest highlights from the St Emlyn's blog and podcast, including the FORCE study, the EXIT study and more about Vitamin C in sepsis...
We hope you enjoy the podcast. Please do like and subscribe on your preferred podcast app and tell your friends and colleagues about us.

Thursday Jun 16, 2022
Ep 202 - May 2022 Round Up
Thursday Jun 16, 2022
Thursday Jun 16, 2022
Our monthly round up of all from the St Emlyn's blog. We discuss pathways into emergency care research, pad positioning in cardioversion of AF and possible gender differences in the presciption of TXA in trauma.
We also chat about travel in Lithuania, memories of defibrillating with hand held paddles and Simon's recent forst infection with COVID.
We mention a post on Lyme disease which you can read here (especially if you live near the New Forest...)

Thursday May 12, 2022
Ep 201 - March/April 2022 Round Up
Thursday May 12, 2022
Thursday May 12, 2022
After a brief hiatus we're back with more from the St Emlyn's Blog. We discuss a wide range of topics from crowding in Emergency Departments and the RePHILL trial to breastfeeding, genetic testing and diagnosing DVTs, as well as our highlights from the recent RCEM CPD Conference in Bournemouth. There really is something for everyone!

Friday Mar 25, 2022
Ep 200 - February 2022 Round Up
Friday Mar 25, 2022
Friday Mar 25, 2022
We made it! A double century of podcasts. In this month's update Iain and Simon talk through myth busting in resuscitation, Rick Body's airway expertise (with a side mention for high sensitivity troponin), a paper about resuscitative thoracotomy, ACPs in EM and how we all could set future research priorties.
Thank you again for listening to the St Emlyn's podcast. We really do hope that you enjoy it and have found our witterings over the last 200 episodes useful.
Hopefully we'll see some of you at the RCEM CPD Conference in Bournemouth next week.
Please do rate us on iTunes, like, subscribe, tweet and tell you friends about the podcast.

Saturday Mar 12, 2022
Ep 199 - Feedback: Update and inter-speciality complexity. St Emlyn’s
Saturday Mar 12, 2022
Saturday Mar 12, 2022
Simon and Natalie discuss some of the complexities of feedback when it involved different specialities and patients. We also review our general rules of feedback.
See https://www.stemlynsblog.org/?s=feedback for more.

Tuesday Feb 22, 2022
Ep 198 - January 2022 Round Up
Tuesday Feb 22, 2022
Tuesday Feb 22, 2022
The first episode of our 9th Season with discussion about Calcium in cardiac arrest, a deep dive into the physiology of exsanguinating haemorrhage, a comparison of ketamine and etomidate for induction of anaesthesia and the ECG Thrust.
Please do like, subscribe and tell your friends about the St Emlyn's podcast.

Friday Jan 14, 2022
Ep 197 - December 2021 Round Up
Friday Jan 14, 2022
Friday Jan 14, 2022
The Season Finale that you've all be waiting for. Our last episode of season 8 includes discussion about racial bias in sats monitoring, CT scans to investigate subarachnoid haemorrhage and the importance of (consensual) touch.
Thanks again for listening. Please like and subscribe and all that. We look forward to seeing you next season (in about a month...)
Iain and Simon

Tuesday Dec 14, 2021
Ep 196 - November 2021 Round Up
Tuesday Dec 14, 2021
Tuesday Dec 14, 2021
Iain is flying solo this month, with discussion about narrative story tellling, airway management in the ED and using pigtail catheters in management of haemothorax.
We hope all you all have a very happy Christmas and chance over the festive period to relax. Do explore our back catalogue of podcasts for more on wellbeing and grief at Christmas.
Please do subscribe and rate and review us on your chosen podcast provider.
Take care all.

Friday Nov 19, 2021
Ep 195 - October 2021 Round Up
Friday Nov 19, 2021
Friday Nov 19, 2021
Our round up of all the blog had to offer in October 2021. There's discussion about evidence based medine in the REST and CTCA for intermediate chest pain trials, more about cauda equina and highlights from the Paediatric Colloquium in Australia, as well as the good humoured chat.
Please see the website for more information and don't forget to subscribe and rate the podcast (if you think it's any good).

Saturday Sep 25, 2021
Ep 194 - August 2021 Round Up
Saturday Sep 25, 2021
Saturday Sep 25, 2021
The round up of the St Emlyn's blog posts in August 2021, featuring discussion about therapeutic anticoagulation in hospitalised COVID-19 patients, non invasive ventilation vs usual care for critically hypoxic COVID-19 patients and the recent EMTA (Emergency Medicine Trainees Association) survey. Oh, and Simon's mid-life crisis.

Sunday Aug 08, 2021
Ep 193 - June and July 2021 Round Up
Sunday Aug 08, 2021
Sunday Aug 08, 2021
Iain and Simon discuss the best from the blog in June and July. There's COVID chat (of course). thunderstorm asthma, a glance into the future and much, much more.

Thursday Jun 17, 2021
Ep 192 - May 2021 Round Up
Thursday Jun 17, 2021
Thursday Jun 17, 2021
It's been a busy month on the blog with plenty for Iain and Simon to talk about. The Manchester Arena bombing, new guidelines for Anaphylaxis management, Adult Congenital Heart Disease, Calcium in Major Haemorrhage and Spontaneous Coronary Artery Dissection all get a mention alongside the usual witterings of two middle aged emergency physicians.

Wednesday May 26, 2021
Ep 191 - Adult Congenital Heart Disease in the ED: Part 2
Wednesday May 26, 2021
Wednesday May 26, 2021
This is the second in a two part podcast series discussing Adult Congenital Heart Disease (ACHD) and how these patients may present to the Emergency Department (ED). Dr Sam Fitzsimmons, our guest on the podcast, is a Consultant in Adult Congenital Heart Disease at University Hospital Southampton. There is more information in this blog post.
In this episode we discuss Eisenmenger Syndrome, Transposition of the Great Arteries and Coarctation of the Aorta.
Thursday May 20, 2021
Ep 190 - Adult Congenital Heart Disease in the ED: Part 1
Thursday May 20, 2021
Thursday May 20, 2021
This is the first in a two part podcast series discussing Adult Congenital Heart Disease (ACHD) and how these patients may present to the Emergency Department (ED). Dr Sam Fitzsimmons, our guest on the podcast, is a Consultant in Adult Congenital Heart Disease at University Hospital Southampton. There is more information in this blog post.
Look out for Part 2, which will be released next week, where we discuss Eisenmenger Syndrome, Transposition of the Great Arteries and Coarctation of the Aorta.
Background
With advances in paediatric cardiac surgery, more and more patients with complex congenital heart disease are surviving to adulthood: in the 1950s you might expect a survival rate of about 10%, whereas now this is more like 85%. In fact, there are more patients in the adult congenital heart disease population than there are in the paediatric one (with 2.3 million adults vs 1.9 million children in Europe).
Many patients with Adult Congenital Heart Disease are young and able to live a relatively normal life. This means that they can travel and take part in just the same sort of activities as those without ACHD. They may well turn up in your Emergency Department one day, regardless of whether you are a tertiary centre or a district general hospital (DGH).
They are experts, and know their disease well, but this does not abstain you from a responsibility to know about them too! When these patients become unwell, they can go downhill very fast and you may not have the chance to discuss with them their exact lesion and its management.
The anatomy and physiology of these patients is abnormal, so they may present in atypical ways, and may not respond to usual medical interventions: in fact, some of our usual treatments may even be harmful.
However, starting with our usual 'ABC' approach is by far the best way to go, whilst gathering more information and contacting their specialist centre. Many patients will have their last clinic letter and ECG with them (which will also have the direct dial number of their specialist). And if they, or their relative, say there is something wrong you must believe them and do all you can to make sure they are fully investigated.
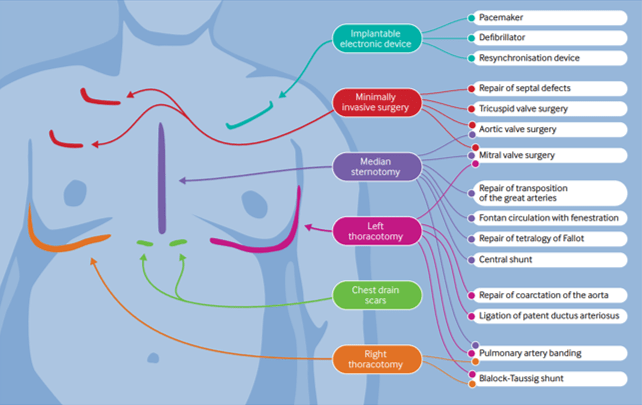
The presence of scars may give you some clues as to the patient's underlying condition and previous surgical repairs. (BMJ 2016; 354: i3905)
A General Approach
- Do your usual ABC assessment.
- Pay particular attention to the respiratory rate - this should be normal.
- Give oxygen if they look unwell.
- They should have a 'normal' blood pressure - any hypotension should be taken as abnormal and investigated.
The Fontan Circulation
This is not a condition in itself, but in fact the resulting circulation after a series of operations that could've been performed due to a number of different underlying conditions:
- Tricuspid Atresia
- Double Inlet Left Ventricle
- Atrio-ventricular Septal Defect – unbalanced
- Pulmonary Atresia
- Hypoplastic Left Heart Syndrome
In essence these patients are born with a single functioning ventricle, that has to be utilised to supply the systemic side of the circulation, whilst the Fontan acts as a passive means of returning blood to the pulmonary circulation.
It was first devised in the early 1970s by Dr Francis Fontan, so the majority of patients with this are in their mid thirties and younger.
Potential reasons for admission to the ED - Fontan circulation
1, Arrythmia
As the patient is entirely dependent on their systemic ventricle to work optimally, any disturbance of the delivery into it is very poorly tolerated. Thus, any arrhythmia is life threatening, even a mild atrial tachycardia.
These patients need to be returned to sinus rhythm as quickly as possible and the recommended method for this is DC cardioversion in expert hands.
Fontan patients have an incredibly fragile circulation and any change in their respiratory physiology can be life threatening, especially if it increases their pulmonary pressures (and thus prevents the passive flow within the Fontan circulation). These patients are not candidates for sedation in the ED and should have an experienced anaesthetist to manage them during the procedure.
Beware if the patient comes in and tells you they are fasted! This means they have been in this situation before and needed DC cardioversion.
2, Haemoptysis
Over time the patient develops venous hypertension within the Fontan connection. This causes the formation of collateral vessels, that may link into the bronchial arterial tree.
If the patient presents in shock treat them as you would any other patient with emergency blood transfusion.
Any haemoptysis, however small, may herald the beginning of a massive bleed. These patients need further investigation, probably a CT chest with contrast. These vessels may then be coiled by interventional radiology.
3, Cyanosis
If the patient has a non fenestrated Fontan they should have normal oxygen saturations. However, if there is a fenestration there will be shunting and therefore a reduction in oxygenation.
For patients this is trade of between being pink or blue, each of which have complications.
Dr Sam Fitzsimmons
Dr Sam Fitzsimmons is a Consultant Cardiologist in Adult Congenital Heart Disease (ACHD) at the University Hospital Southampton, UK. Sam also subspecialises in pulmonary hypertension and maternal cardiology. Working within a tertiary surgical ACHD centre, Sam delivers an ACHD on call service for emergency admissions, inpatient care, routine outpatient follow-up, intra-operative imaging and post-surgical care, as well as specialist clinics in Pulmonary Hypertension and Maternal Cardiology. Sam holds a Honorary Senior Clinical Lecturer post with the University of Southampton as she is passionate about teaching and in particular, she is enthusiastic about helping demystify congenital heart disease for many non-specialist to improve patient care. Sam is well published in peer review journals, cardiology textbooks and specialist guidelines.

Friday May 14, 2021
Ep 189 - April 2021 Round Up
Friday May 14, 2021
Friday May 14, 2021
A podcast with Iain and Simon summarising all the latest content from the St Emlyn's blog in April 2021. Topics discussed include Vaccine Induced Thrombocytopenic Thrombosis, how our own biases can effect our critical appraisal and whether we need to worry about grading the quality of FOAMed resources.
Thanks for listening. Please check out the blogs themselevs at www.stemlynsblog.org and consider subscribing and rating us on iTunes.
If you'd like to see some more from Peter Brindley you can watch one of his SMACC talks here.

Thursday May 06, 2021
Ep 188 - India COVID19 wave in Spring 2021
Thursday May 06, 2021
Thursday May 06, 2021
Simon joins Ankur Verma from Delhi, to talk about the impact of COVID in the latest wave devastating India.

Sunday Apr 11, 2021
Ep 187 - March 2021 Round Up
Sunday Apr 11, 2021
Sunday Apr 11, 2021
A discussion about all the latest from the St Emlyn's blog, including a hot off the press article about vaccine induced thrombocytopenic thrombosis and the new FRCEM revision guide.
Simon and Iain also talk about the latest results from the RECOVERY trial, Major Trauma Triage tools, cricothyroidotomy, thromboprophylaxis in COVID19 and the new Medical Licensing Assessment for medical students and the new St Emlyn's Undergraduate Curriculum

Thursday Apr 08, 2021
Ep 186 - Assessing online medical education resources with Peter Brindley
Thursday Apr 08, 2021
Thursday Apr 08, 2021
An audio review of a paper in the Journal of Intensive Care Medicine with two of the authors.
Assessing on-line medical education resources: A primer for acute care medical professionals and others
Peter G Brindley, Leon Byker, Simon Carley, Brent Thoma https://doi.org/10.1177/1751143721999949

Monday Mar 15, 2021
Ep 185 - February 2021 Round Up
Monday Mar 15, 2021
Monday Mar 15, 2021
Our regular podcast round up from February 2021. Iain and Simon highlight the key learning points from this month on the St Emlyn’s blog and podcast.
Topics discussed this month include tocilizumab in COVID19, TIA risk scores, new Emergency Care standards (targets) and TXA use in epistaxis. We also pay tribute to Dr Cliff Mann, former President of RCEM who sadly died this month.
Please remember to subscribe to the podcast on iTunes/Google Play and please do leave us some reviews and ratings there.

Saturday Feb 20, 2021
Ep 184 - January 2021 Round Up
Saturday Feb 20, 2021
Saturday Feb 20, 2021
Our regular round up of the best of the blog and podcast from January 2021 with Iain and Simon. The St Emlyn's blog posts from January 2021 are discussed, including plenty about Coronavirus as well as other topics relevant to anyone interested in Emergency Medicine and evidence based care.

Thursday Feb 18, 2021
Thursday Feb 18, 2021
Going into hospital as an emergency during the COVID-19 pandemic must be extremely scary for patients and their relatives. With no relatives allowed to visit and staff dressed in full PPE, the experience must be so much more unnerving than usual. Add to that the incredible worry about catching COVID-19 for those who don’t already have it; or the worry about what might happen for those who do. Will they pull through? Could this be the end?
I’m privileged to be co-leading the COvid-19 National DiagnOstic Research and evaluation programme (CONDOR), which involves a collaboration between amazing teams in Manchester, Oxford, Leeds, Newcastle, London and Nottingham. The programme evaluates diagnostic tests for COVID-19.
We’re extremely lucky to have two very experienced and proactive patient and public representatives as members of our steering committee: Graham Prestwich from Leeds and Val Tate from Oxford.
I recently spoke with Graham and Val to get their thoughts about how we, as clinicians, might effectively communicate with patients during the COVID-19 pandemic. They provide their important insights from a lay perpsective about what they would want from their clinician.
We cover everything from the challenges of communicating while wearing PPE to the way to answer important questions like, “Am I going to die?”, which many of us have, I’m sure, had to answer on a number of occasions over the past 12 months.
I hope that you enjoy the podcast. We realise that 25 minutes wasn’t long enough to cover everything we’d have liked to.We’d really like to know what you think. Are there things that we haven’t covered that you’d like us to? What are your experiences? We’d love you to share your thoughts in the chat!
Rick

Sunday Jan 17, 2021
Ep 182 - COVID-19 vaccines update (January 2021)
Sunday Jan 17, 2021
Sunday Jan 17, 2021
A vaccine update with Rick Body, Simon Carley, Pam Vallely, Paul Klapper and Charlie Reynard. Bringing RCEM, St Emlyn's and the University of Manchester together for the latest thoughts and wisdom on the vaccines that might get us out of this pandemic.
Moderna vaccine phase 3 trial - https://www.nejm.org/doi/full/10.1056/nejmoa2022483
Oxford vaccine phase 2/3 - https://www.thelancet.com/pdfs/journals/lancet/PIIS0140-6736(20)32466-1.pdf
Pfizer vaccine trial - https://www.nejm.org/doi/full/10.1056/NEJMoa2034577
#vaccines #COVID19 #coronavirus

Thursday Dec 17, 2020
Ep 181 - Christmas 2020 Round Up
Thursday Dec 17, 2020
Thursday Dec 17, 2020
A special festive edition of our round up podcast featuring six weeks of blog posts and plenty more besides.
From all at St Emlyn's we hope you have a very happy festive season and we cannot wait to talk to you again in 2021.
Take care,
Simon and all the team

Friday Nov 27, 2020
Friday Nov 27, 2020
Rick leads the FALCON and CONDOR studies that are currently evaluating COVID-19 studies in the UK. Nobody knows more about how we can practically use COVID-19 testing than Rick and in this podcast he takes us through what is available and how we might use it in the future.
A great listen and lots to learn.

Friday Nov 06, 2020
Ep 179 - October 2020 Round Up
Friday Nov 06, 2020
Friday Nov 06, 2020
A bumper edition of the podcast where Iain and Simon discuss TXA (twice), antibiotics in appendicits, VTE, Blood products in trauma, use of ultrasound in cardiac arrest and plasma in traumatic brain injury. Oh, and COVID19 (but not for long)...
An evidence based cornucopia of aural pleasure.
Please like and subscribe (as all podcasters seem to say).
Take care,
Iain

Saturday Oct 24, 2020
Ep 178 - Surviving the Second Wave with Liz Crowe (October 2020)
Saturday Oct 24, 2020
Saturday Oct 24, 2020
In this special edition of the podcast, Liz Crowe discusses with Iain how we can find contentment, despite the relentless nature of COVID19 and the impending second wave. She gives practical, realistic advice that everyone can consider and encourages us all to be kind to ourselves in these strange and difficult times.

Tuesday Oct 20, 2020
Ep 177 - September 2020 Round Up
Tuesday Oct 20, 2020
Tuesday Oct 20, 2020
Welcome to our audio round up of everything on the blog during September.
It's been a relatively quiet on the blog post this month, but we chat through not only blogposts on the REMAP-CAP trial, TXA in Head Injury and the ISARIC COVID Risk prediction tool, but also the situation in the North of England and the recent RCEM Virtual Conference.
The numbers of Lesson Plans available continue to grow. We've had some great feedback following their use in induction. If tyou've not seen them yet, do have a look and let us know what you think. If you're interesed in learning more about Baysian thinking this Lesson Plan is a good place to start.
Take care,

Thursday Oct 01, 2020
Ep 176 - JC: Can we give tranexamic acid (TXA) via the IM route? (October 2020)
Thursday Oct 01, 2020
Thursday Oct 01, 2020
Interview with Ian Roberts on the pharmacokinetic trial of intramuscular tranexamic acid.
Blog link here

Thursday Sep 10, 2020
Ep 175 - August 2020 Round Up
Thursday Sep 10, 2020
Thursday Sep 10, 2020
Welcome to our audio round up of everything on the blog during August.
As the world continues to be in the grips of the Coronavirus pandemic there have been more papers looking at all aspects of this disease.
Simon reviewed the latest paper on Hydroxychloroquine and Charlie collated some of the top papers covering aspects from aerosol spread and use of CPAP to the effect on vulnerable groups and the effect on staff psychological health
It's not all COVID though. Sepsis is a condition we all want to be able to treat more effectively. Sadly there doesn't seem to be any encouraging news about the use of Vitamin C, Steroids and Thiamine in this latest RCT.
Many of the St Emlyn's group have special expertise in toxicology and Gareth wrote this incredibly informative post about the use of GBL. If you're not sure what "ChemSex" is then this post from a few years ago by Janos is worth a read.
The anonymously written "Look at what they make you give" post really struck a chord with readers, with an astonishing number of views. There are messages here for us all.
The numbers of Lesson Plans available continue to grow. We've had some great feedback following their use in induction. If tyou've not seen them yet, do have a look and let us know what you think.

Saturday Aug 01, 2020
Ep 174 - June and July 2020 Round Up
Saturday Aug 01, 2020
Saturday Aug 01, 2020
Our own version of Buy One Get One Free* this month, where you get a round up of two months of blog content.
Coronavirus continues to dominate the medical (and non-medical) headlines, and we discuss the two major results from the RECOVERY trial published recently, one positive and one not so (depending on who you talk to....). Simon also catches up with Roberto Cosentini, who you'll remember from the very powerful podcast at the beginning of the pandemic.
COVID isn't the only EBM circus in town though: we've reviewed HALT-IT and Simon has given a talk about the "Ten Top Trauma Papers" of the last year and Laura reviewed a paper looking at haloperidol for headaches.
We're having to think even harder about how we communicate in the ED, both for clinical care and to deliver education. Two ideas to help learning have been featured this month: The St Emlyn's Lesson Plans and "Background Learning".
Good luck to all those starting in Emergency Medicine, and a huge thank you to all those who are moving to other areas of medicine or other departments. It's been a curious few months...
Take care,
Iain
*It's actually Get One Free Get Another Free, but whose ever heard of that?
Thursday Jun 25, 2020
Ep 173 - The St Emlyn's Lesson Plans
Thursday Jun 25, 2020
Thursday Jun 25, 2020
We are delighted to introduce you to the "St Emlyn's Lesson Plans", which we hope will help structure some of your education sessions over coming months (and years).
Each lesson plan starts with a descrete learning outcome, to set the scene, as well as details of the RCEM curriculum item(s) that will be covered.
The first tasks are aimed at aquiring some background knowledge and can either be done as part of the session, or beforehand. These utilise the vast "FOAMed" resources (including, but not exclusively, those of St Emlyn's).
Our experience is that time constraints often mean that "background reading" isn't achieved before the session, so would encourage allowing time within it to complete these. They are designed to take about 30 minutes and occupy the first half of the session.
Everything you need for each lesson is included in the plan. We would recommend that each learner has an internet enabled device available (with headphones) to read and listen to the background material at their own pace.
The second half of the session should be facilitated by an expert. This can happen in person, but also online, via any of the interfaces that are now so familiar.
In many plans we have given some case examples, but it would be even better if learners can bring cases of their own for discussion. This element is very much within the control of the facilitator (who should been fully cogniscent of the contents of the knowledge section).
The session finishes off with a summary, this should emphasise again the most important learning points. To really embed the knowledge and skills the particiapants should be encouraged to reflect on what they have learned, and to even talk to thse who were unable to attend about what they missed.
For learners this also gives an opportunity to easily link teaching sessions to their portfolio.
You may want to record the "face-to-face" elements, so that those who were not present are able to access them when they can (and those that did can rewatch to refresh their learning).
Although these plans are designed for delivery in a single centre, there is absolutely no reason why regional (or even national) teaching could take place in this way. The recent COVID19 Journal Clubs have demonstrated beautifully how a group of learners can engage with an online panel.
We would be very happy to receive lessons plans to add to the collection. This is very much a collaborative effort.
Please let us know what you think of these lesson plans and if you are using them in your Department. We'd love to hear your ideas about how we can take medical education forward.

Friday Jun 19, 2020
Ep 172 - Dexamethasone and COVID - Show us the Data! (June 2020)
Friday Jun 19, 2020
Friday Jun 19, 2020
St Emlyn's three professors, Carley, Body and Horner* critically appraise the Press Release regarding Dexamethasone in the treatment of COVID-19.
What does this mean for the future of Evidence Based Medicine? Can we really start using a medication when the trial hasn't been peer reviewed and the full dataset not released?
The blog post by Josh Farkas, that is mentioned in the podcast, is here.
*Professor Simon Carley, Professor of Emergency Medicine at Manchester Metropolitan University and a Consultant in Adult and Paediatric Emergency Medicine at Manchester Foundation Trust, Professor Rick Body Professor of Emergency Medicine in Manchester and Honorary Consultant in Emergency Medicine at Manchester Foundation Trust. Professor Dan Horner, Professor of Emergency Medicine of the Royal College of Emergency Medicine and Consultant in Emergency Medicine and Intensive Care at Salford Royal NHS Foundation Trust.

Saturday Jun 13, 2020
Ep 171 - May 2020 Round Up
Saturday Jun 13, 2020
Saturday Jun 13, 2020
Lots to chat about on the podcast this month, and not just COVID! There's been blog posts about clots, troponin and even telly, as well as the Journal Club series.
Keep a look out for the new St Emlyn's Lesson Plans that we hope will help usher in a new era of medical education in a socially distanced world.
If you would like to donate to the fund in the memory Adel Aziz you can find the link here.
We hope you're finding all of our output useful. Please do subscribe to the website (in the top right hand corner) and rate our podcast on iTunes.
Take care
Iain
Podcast edited by Izzy Carley
PS You can find the Lesson Plans here. Still a work in progress, but as you've read these "shownotes" you deserve to have a sneak preview...
