
1.3M
Downloads
288
Episodes
A UK based Emergency Medicine podcast for anyone who works in emergency care. The St Emlyn ’s team are all passionate educators and clinicians who strive to bring you the best evidence based education. Our four pillars of learning are evidence-based medicine, clinical excellence, personal development and the philosophical overview of emergency care. We have a strong academic faculty and reputation for high quality education presented through multimedia platforms and articles. St Emlyn’s is a name given to a fictionalised emergency care system. This online clinical space is designed to allow clinical care to be discussed without compromising the safety or confidentiality of patients or clinicians.
A UK based Emergency Medicine podcast for anyone who works in emergency care. The St Emlyn ’s team are all passionate educators and clinicians who strive to bring you the best evidence based education. Our four pillars of learning are evidence-based medicine, clinical excellence, personal development and the philosophical overview of emergency care. We have a strong academic faculty and reputation for high quality education presented through multimedia platforms and articles. St Emlyn’s is a name given to a fictionalised emergency care system. This online clinical space is designed to allow clinical care to be discussed without compromising the safety or confidentiality of patients or clinicians.
Episodes

Saturday Jan 14, 2017
Ep 87 - Critical Appraisal Nugget 6: Retrospective and Prospective studies
Saturday Jan 14, 2017
Saturday Jan 14, 2017
Understanding Prospective and Retrospective Studies: Key Differences, Advantages, and Applications
In the field of medical research, the distinction between prospective and retrospective studies is fundamental. These study designs differ primarily in the timing of data collection relative to the occurrence of outcomes, which significantly influences the quality, reliability, and applicability of the research findings. This detailed exploration aims to elucidate the characteristics, strengths, and limitations of each design, offering practical insights into their use in clinical research and practice.
Defining Prospective and Retrospective Studies
Prospective Studies involve the identification and enrollment of participants before the outcomes of interest occur. This design allows researchers to follow participants over time, observing events as they happen. For instance, in a study focused on chest pain, researchers would enrol patients at the onset of symptoms and monitor them to see if they develop conditions like myocardial infarction (MI). The prospective nature of these studies provides a structured approach to data collection, ensuring that all relevant information is captured consistently.
Retrospective Studies, conversely, involve examining existing data after the outcomes have occurred. In this design, researchers typically review medical records or databases to identify patients who have experienced specific events, such as an MI, and then analyze these records to explore potential risk factors or causes. This approach is often more efficient and less costly than prospective studies, as it utilizes data that have already been collected.
Key Differences Between Prospective and Retrospective Studies
The timing of data collection in relation to the occurrence of outcomes is a critical differentiator between these study designs. This temporal aspect influences several key factors, including data quality, potential biases, and the strength of causal inferences that can be drawn.
Data Collection and Quality
One of the primary advantages of prospective studies is the ability to standardize data collection. Since the data is collected in real-time, researchers can establish clear protocols for what data to collect and how to collect it. This reduces variability and enhances the reliability of the study findings. For example, in a prospective study on hypertension, researchers can use a standardized checklist to document whether each participant has hypertension, ensuring consistent and accurate data across all participants.
In contrast, retrospective studies depend on the quality and completeness of existing records, which were often not compiled with the current research question in mind. This reliance on historical data can lead to inconsistencies and gaps. For instance, a patient's medical record might not specify whether they had hypertension, either because it was not asked about or not documented. Such missing data can lead to biases and affect the study's conclusions, as the researchers may not have all the necessary information to make accurate assessments.
Timing and Outcome Identification
In prospective studies, participants are observed from the point of exposure or initial symptoms to the outcome, allowing researchers to track changes over time and potentially identify causative factors. This direct observation of the sequence of events enhances the ability to establish a cause-and-effect relationship. For instance, if a prospective study monitors patients presenting with chest pain, it can track the development of MI, thereby strengthening the evidence for an association between initial symptoms and outcomes.
Retrospective studies, however, start with the outcome and work backwards to explore potential causes. This backwards-looking approach can introduce recall bias and selection bias, as the outcomes are already known and may influence which data are emphasized or selected. Additionally, retrospective studies are constrained by the availability and accuracy of past records, which can vary widely and may not cover all variables of interest, potentially leading to incomplete or skewed data.
Advantages and Limitations of Each Study Design
Both prospective and retrospective studies offer unique benefits and face distinct challenges, making them suitable for different types of research questions and practical considerations.
Prospective Studies
Advantages:
- High Data Quality: Prospective studies allow for systematic and standardized data collection, minimizing the risk of missing or incomplete data.
- Causal Inference: The temporal relationship between variables and outcomes can be clearly established, supporting stronger causal inferences.
- Real-Time Data Collection: Researchers can monitor the study as it progresses, allowing for adjustments to data collection methods if new relevant variables emerge.
Limitations:
- Resource-Intensive: Prospective studies often require significant time, financial investment, and effort. The need for long-term follow-up can be particularly demanding.
- Long Duration: These studies can take years to complete, especially for conditions with long latency periods, delaying the availability of results.
- Participant Dropout: Over extended periods, there is a higher risk of participant dropout, which can reduce the study's validity and potentially bias the results.
Retrospective Studies
Advantages:
- Efficiency: Retrospective studies can be conducted relatively quickly since they rely on already available data.
- Lower Cost: The use of existing records reduces the need for expensive data collection processes, making these studies more cost-effective.
- Feasibility for Rare Conditions: Retrospective studies are particularly useful for examining rare conditions or outcomes that would require a prohibitively large cohort in a prospective design.
Limitations:
- Data Quality Issues: Relying on existing records can lead to inconsistent data quality, with gaps or inaccuracies potentially affecting the study's findings.
- Bias: These studies' retrospective nature can introduce biases, such as selection bias and information bias, that can compromise the validity of the results.
- Limited Causal Inference: Establishing a cause-and-effect relationship is more challenging due to the lack of temporal clarity between exposure and outcome.
Practical Application in Medical Research and Practice
Understanding the strengths and weaknesses of prospective and retrospective studies is essential for effectively interpreting medical literature and applying research findings in clinical settings. For example, a study evaluating the effectiveness of a diagnostic tool for acute coronary syndrome would be assessed differently depending on whether it was conducted prospectively or retrospectively.
Prospective studies are often regarded as the gold standard for clinical trials, particularly when testing new treatments or interventions. Their ability to minimize bias and control for confounding variables makes them invaluable for determining efficacy and safety. However, the high cost and time requirements can be significant barriers, especially in large-scale studies or those requiring long-term follow-up.
While not as robust in establishing causality, retrospective studies are highly valuable for exploring existing data and generating hypotheses. They are especially useful in situations where prospective studies are impractical due to ethical concerns, time constraints, or the rarity of the condition being studied. For instance, retrospective analyses of patient records can provide insights into the natural history of a disease or the effectiveness of treatments in real-world settings.
Case Study: Evaluating the HEART Score
The HEART score, a tool used in emergency departments to risk stratify patients with chest pain, serves as an illustrative example of the application of these study designs.
In a prospective study, researchers would enrol patients presenting with chest pain and systematically apply the HEART score, following these patients over time to track outcomes such as MI or other adverse cardiac events. This prospective approach allows for a controlled and consistent application of the score, with data collected in real time. Researchers can ensure that all relevant factors, such as patient history and troponin levels, are accurately recorded, providing a clear picture of the score's predictive value.
In a retrospective study, researchers might review existing medical records of patients who presented with chest pain and were tested for troponins. They would calculate the HEART score based on the available data and correlate it with documented outcomes. While this method is more efficient and cost-effective, it is limited by the quality of the records. Incomplete or inaccurately recorded data, such as missing details on patient history, can affect the accuracy of the HEART score's evaluation, potentially leading to less reliable conclusions.
Ethical Considerations
Ethical considerations differ significantly between prospective and retrospective studies. Prospective studies often require informed consent from participants, as they involve collecting new data. This process ensures that participants are aware of the study's purpose, procedures, and potential risks, and they have the right to withdraw at any time. However, obtaining consent can be challenging in emergency settings or when the study involves vulnerable populations.
Retrospective studies typically use anonymized data, which simplifies ethical considerations by removing the need for consent. This approach is particularly advantageous when dealing with sensitive information, as it protects patient privacy and confidentiality. However, researchers must still ensure that data are used responsibly and that individuals' privacy is not compromised. The use of anonymized data also limits the ability to collect additional information that may be relevant to the study but was not included in the original records.
Conclusion: Choosing the Right Study Design
The decision between using a prospective or retrospective study design should be guided by the research question, available resources, and the specific context of the study. Each design offers unique benefits and challenges, and the choice will impact the strength and applicability of the findings.
Prospective studies are preferred when high-quality data and strong causal inferences are needed, despite their higher costs and time requirements. They are ideal for intervention studies, where controlling for confounding factors is crucial.
While limited in establishing causality, retrospective studies provide valuable insights when prospective studies are not feasible. They are particularly useful for exploring existing data, understanding the epidemiology of diseases, and identifying potential risk factors.
In clinical practice, understanding these differences helps healthcare professionals critically appraise the literature, making informed decisions based on the strengths and limitations of the evidence. At St Emlyn's, we emphasize the importance of critical appraisal and evidence-based practice. By familiarizing yourself with these study designs, you can enhance your ability to interpret research findings, apply them in clinical settings, and contribute to the ongoing advancement of medical knowledge.
Thank you for exploring the complexities of prospective and retrospective studies with us. We hope this detailed discussion has provided clarity and practical guidance, empowering you to approach medical research with a critical and informed perspective. For more in-depth analysis and practical insights, continue following St Emlyn's, your trusted source for cutting-edge medical education and research.
Friday Jan 06, 2017
Ep 86 - Critical Appraisal Nugget 5: Journal Clubs
Friday Jan 06, 2017
Friday Jan 06, 2017
Setting up a really great journal club.

Tuesday Dec 13, 2016
Ep 85 - Top tips for chest drains.
Tuesday Dec 13, 2016
Tuesday Dec 13, 2016
Title: Mastering Chest Drains: Essential Tips and Techniques for Emergency Medicine
In this comprehensive guide, Simon Carley and Rick Bodey from St Emlyns explore the essential aspects of chest drains, also known as intercostal drains or chest tubes, focusing on their importance, optimal techniques, and common pitfalls in emergency medicine.
Importance of Chest Drains
Chest drains are critical for managing conditions like pneumothorax, hemothorax, and pleural effusion by removing air, blood, or fluid from the pleural cavity. Despite not being a daily procedure in the UK, proficiency in chest drain insertion is crucial due to the potential for severe complications, including organ damage and infection. Proper training and careful execution are necessary, especially as new technologies and medical practices evolve.
Choosing the Right Size
Traditionally, large-bore drains (32-36 French) were used for pneumothoraces to prevent blockage by clots. However, recent evidence supports the use of smaller drains (28-32 French), even for trauma patients. Smaller drains are less invasive, cause less discomfort, and are equally effective. The move towards smaller drains aligns with a trend in medicine favoring minimally invasive procedures, which reduce patient risk and enhance comfort.
Management of Occult Pneumothoraces
Advances in imaging, like CT scans and ultrasound, have increased the detection of occult pneumothoraces, which are often asymptomatic and not visible on chest x-rays. Traditional guidelines recommended chest drains for all traumatic pneumothoraces, but recent research suggests conservative management may be appropriate in many cases. A systematic review found no significant difference in outcomes between patients with occult pneumothoraces managed conservatively and those who received chest drains. This highlights the importance of assessing each patient's condition, monitoring closely, and only intervening when necessary, particularly in stable, asymptomatic patients.
Optimizing Analgesia
Pain management during chest drain insertion is vital. Traditional local anesthesia methods are often insufficient, especially in trauma settings. Ketamine has emerged as an effective option, providing both analgesia and sedation without significant respiratory depression. Administered in small, incremental doses, ketamine helps manage pain and anxiety, making the procedure more tolerable. Additional analgesics, like fentanyl and midazolam, can complement ketamine, offering a multimodal approach to pain management.
Intra-Pleural Analgesia
Injecting local anesthetics, such as bupivacaine, into the pleural cavity can further enhance patient comfort, particularly as the lung re-expands and contacts the parietal pleura. This method is supported by randomized controlled trials and can significantly reduce pain in the first few hours post-insertion, aiding in better respiratory function and reducing the risk of complications like pneumonia.
Securing the Drain
Properly securing the chest drain is crucial to prevent accidental dislodgement, especially during patient transport or imaging. Techniques like Neil Bandari's "Jo'burg knot" offer reliable methods for securing drains, though simpler techniques may suffice for less frequent practitioners. Transparent dressings are recommended to allow monitoring of the insertion site and ensure the drain remains securely anchored.
The Role of Ultrasound
Ultrasound is an invaluable tool for accurately placing chest drains, particularly in cases of pleural effusion or complex pleural anatomy. It aids in identifying the best insertion site, reducing the risk of complications, and confirming the resolution of pneumothorax. Ultrasound is especially useful in patients with obesity or chronic lung conditions, where traditional landmarks may not be reliable.
Aspiration of Pneumothoraces
For primary spontaneous pneumothoraces, aspiration may be a viable alternative to chest drain insertion, particularly when specific criteria are met. This less invasive approach can be performed with a standard IV cannula or a small Seldinger technique, which also provides a pathway for chest drain insertion if necessary. This method is beneficial in outpatient settings, allowing for quick resolution without hospitalization.
Conclusion
The management of chest drains is a dynamic field, continually evolving with new research and technology. Emergency medicine practitioners must stay informed and adapt to evidence-based practices, including the use of smaller chest drains, conservative management of occult pneumothoraces, optimized analgesia, and the application of ultrasound. The goal is to provide safe, effective, and patient-centered care, minimizing unnecessary interventions.
At St Emlyns, we strive to share knowledge and best practices to enhance patient care. We invite our readers to contribute their insights and experiences, fostering a collaborative approach to improving clinical skills and outcomes in emergency medicine.

Friday Dec 09, 2016
Ep 84 - Critical Appraisal Nugget 4: Intention to Treat
Friday Dec 09, 2016
Friday Dec 09, 2016
Understanding Intention to Treat in Clinical Trials: A Key Concept for Critical Appraisal
Welcome to the St Emlyns podcast! In this episode, Simon Carley and Rick Bodey delve into an essential topic for anyone interested in critical appraisal and clinical trials—Intention to Treat (ITT). This principle is a cornerstone in the analysis of randomized controlled trials (RCTs), crucial for ensuring the validity and applicability of study findings.
What is Intention to Treat (ITT)?
ITT is a methodological principle used in the analysis of data from RCTs. It requires that participants be analyzed in the groups to which they were originally randomized, regardless of whether they adhered to the treatment protocol. This approach helps maintain the benefits of randomization, such as comparability between groups, and provides a more conservative and realistic estimate of a treatment's effectiveness.
The ITT principle is essential because it preserves the randomization process's integrity, ensuring that the groups remain comparable. This comparability helps minimize bias, allowing researchers to attribute differences in outcomes to the interventions rather than to other confounding factors.
Importance of ITT in Clinical Trials
The ITT principle plays a critical role in RCTs by ensuring that the analysis reflects real-world scenarios where patients may not perfectly adhere to treatment regimens. For example, in a trial comparing a new anticoagulant, Carleyoxaban, to warfarin, ITT analysis would include all participants, even those who did not complete the treatment due to side effects. This comprehensive approach provides a more accurate reflection of the treatment's potential benefits and risks in everyday clinical practice.
By including all participants as originally allocated, ITT analysis helps prevent bias introduced by excluding participants who experience adverse effects or switch treatments. This is vital for obtaining a realistic estimate of the treatment's effect, considering real-world complexities such as patient non-compliance.
Challenges and Considerations
While ITT is the gold standard for RCT analysis, it does come with challenges. One significant challenge is that it can obscure the reasons why participants dropped out or switched treatments. These reasons can provide valuable insights into the treatment's tolerability and feasibility. For instance, in the hypothetical trial with Carleyoxaban, understanding why 50% of participants dropped out could highlight serious side effects that might not be evident from an ITT analysis alone.
In some cases, a per-protocol analysis, which includes only those participants who fully adhered to the treatment protocol, can offer additional insights. This type of analysis can help distinguish between a treatment's efficacy (its effect under ideal conditions) and effectiveness (its effect in a typical clinical setting). However, per-protocol analysis can introduce bias by including only those who were more likely to tolerate and benefit from the treatment.
ITT vs. Per-Protocol Analysis
Per-protocol analysis is particularly valuable in certain situations, such as non-inferiority trials. These trials aim to show that a new treatment is not worse than an existing one. In such cases, per-protocol analysis can provide a more conservative estimate, ensuring that observed differences are not due to adherence variations between groups.
For example, in a trial evaluating a new protocol for early discharge of patients with suspected pulmonary embolism, ITT might show no difference in outcomes if many participants did not follow the new protocol. However, a per-protocol analysis could reveal whether the protocol, when followed, led to improved outcomes or safety concerns.
Similarly, in trials assessing new medications, ITT can provide a realistic estimate by accounting for dropouts due to side effects. This is crucial for understanding the medication's overall safety and effectiveness in the general population.
Practical Implications for Clinicians
For clinicians, understanding ITT is essential for interpreting the results of clinical trials. ITT analysis offers a pragmatic view of a treatment's potential benefits and risks, reflecting the complexities of real-world clinical practice. When deciding whether to use a new treatment, clinicians must consider factors like patient adherence and potential side effects, both of which are accounted for in ITT analyses.
Moreover, clinicians should be critical when appraising studies, checking whether ITT principles were followed. This includes examining flow diagrams that show participant allocation and follow-up, ensuring that the number of participants analyzed matches those initially randomized. Such diligence helps ensure that study findings are robust and applicable to clinical practice.
Conclusion and Key Takeaways
-
ITT is Essential: It preserves the benefits of randomization and provides a realistic estimate of treatment effects by including all participants as initially allocated.
-
Per-Protocol Analysis: While useful in certain contexts, such as non-inferiority trials, it should be interpreted cautiously due to potential biases.
-
Real-World Relevance: ITT helps clinicians understand the applicability of trial results in everyday practice, considering issues like non-compliance and side effects.
-
Critical Appraisal: Clinicians should always verify if ITT analysis was performed when appraising studies, as it ensures a comprehensive understanding of the treatment's effectiveness.
As we continue to explore critical appraisal and clinical trials, we encourage you to stay tuned to the St Emlyns podcast. Future episodes will delve deeper into various aspects of clinical research, providing valuable insights to enhance your practice. Understanding concepts like ITT not only improves your ability to interpret research but also equips you with the tools to make informed, evidence-based decisions in patient care.
Thank you for joining us in this discussion. The ITT principle is a key component of high-quality RCTs and an essential concept for anyone involved in clinical research or patient care. By mastering this and other critical appraisal tools, you can significantly improve your understanding of medical literature and contribute to better patient outcomes. Stay curious, keep learning, and we'll see you in the next episode of the St Emlyns podcast!

Thursday Nov 17, 2016
Ep 83 - The Teaching Course in NYC Round Up
Thursday Nov 17, 2016
Thursday Nov 17, 2016
Insights from the New York Teaching Course: Enhancing Medical Education
Welcome to the St. Emlyn's blog! I'm Iain Beardsell, sharing insights from the recent New York Teaching Course, an event organized by Rob Rogers and Saline Rissai. This course brought together educators from diverse backgrounds, including pediatric surgeons, flight nurses, PhD students, and even a veterinarian, all united by the goal of becoming better educators. Notable attendees included Ross Fischer, Ashley Leibig, Sandra Viggers, and Camilla Sauronson, who shared their experiences and key takeaways.
Diverse Expertise and Shared Learning
The New York Teaching Course offered a unique opportunity to learn from a broad spectrum of expertise. Ross Fischer, a Pediatric Surgeon and presentation expert, found it humbling to be sought after for his advice on presentation skills. He highlighted the importance of continual improvement, noting the evolution of presentations over the years. His blog, ffoliet.com, offers valuable tips for enhancing presentation skills, a crucial aspect of effective teaching.
Ashley Leibig, known for her contributions to St. Emlyn's and her work at SMAC, emphasized the value of open communication. She appreciated the honesty in feedback sessions, where participants openly shared their past errors and positive feedback practices. This openness is essential for professional growth and creating a safe learning environment.
Sandra Viggers, a research fellow at the Copenhagen Academy for Medical Education and Simulation, focused on the power of vulnerability in simulation and debriefing. She found the social events particularly impactful, highlighting a moment where a participant shared a personal story, moving many to tears. This reinforced the importance of sharing and building a supportive community in educational settings.
Camilla Sauronson, a medical student from Denmark and PhD candidate in Tourette Syndrome, valued the inspiring environment of the course. She was particularly interested in innovative teaching methods like the flipped classroom, which involves engaging learners with materials before group discussions. This method fosters active learning and deeper understanding, a shift from traditional lecture-based teaching.
Key Takeaways and Learning Points
The course provided numerous valuable insights and practical lessons:
-
Flipped Classroom: Camilla Sauronson emphasized the effectiveness of the flipped classroom approach, which encourages students to engage with educational content before attending group discussions. This method promotes active learning and enriches classroom interactions.
-
Constructive Feedback: The feedback session led by George Willis was a highlight, demonstrating the importance of giving constructive feedback. Ashley Leibig noted the challenges in providing good feedback but appreciated the practical pointers provided during the session. Effective feedback is critical for personal and professional development.
-
Presentation Skills: Ross Fischer underscored the continuous need to refine presentation skills. His insights into slide design and delivery were invaluable, reminding educators of the importance of clear and engaging communication in teaching.
-
Resilience and Wellbeing: Sandra Viggers reflected on Chris Doty's talk on resilience. Doty discussed recognizing signs of burnout and the importance of self-care. Sandra emphasized the need for educators to be mindful of their own and their learners' wellbeing, highlighting the role of supportive relationships in preventing burnout.
-
Engaging Lectures: Ken Mills' interactive workshop on evidence-based medicine showcased that lectures can be both educational and entertaining. Using historical figures to illustrate concepts made the session memorable and engaging, demonstrating that education can and should be enjoyable.
Building a Supportive Educational Community
A particularly poignant moment during the course was a participant sharing a deeply personal story during a social event. Sandra Viggers emphasized the significance of vulnerability and the supportive community fostered at the course. This sense of community is vital in emergency medicine and education, where the pressures of the job can be intense. Building strong, supportive networks helps individuals navigate challenges and grow both personally and professionally.
Practical Applications and Future Directions
As the course concluded, participants were encouraged to apply what they had learned in their own teaching practices. Key practical steps include:
- Implementing the Flipped Classroom: Start by incorporating pre-session materials like podcasts or articles, fostering richer discussions during group sessions.
- Developing Effective Feedback Techniques: Create a structured approach to giving feedback, focusing on being constructive and empathetic.
- Enhancing Presentation Skills: Regularly review and improve presentation materials, seeking feedback from peers.
- Prioritizing Wellbeing: Integrate wellbeing discussions into educational curricula and encourage self-care practices among staff and students.
- Fostering a Supportive Community: Create opportunities for personal sharing and team-building, strengthening trust and collaboration.
Looking Forward
The New York Teaching Course was an enriching experience, and similar events are planned for the future, including one in Copenhagen before the next SMAC conference. These courses provide more than just educational content; they are opportunities to connect with a global community of educators dedicated to improving their craft.
For more detailed reflections and session summaries, the Scan FOAM website offers comprehensive coverage. Their posts provide a virtual experience of the course, nearly as immersive as attending in person.
Conclusion: A Commitment to Continuous Improvement
The New York Teaching Course reinforced that teaching is not merely about imparting knowledge but about connecting with students, being vulnerable, and continuously improving. Whether you're an experienced educator or just starting, there's always room for growth. Let's carry forward the lessons learned, strive to be better educators, and support our students and colleagues. Thank you for joining us on this journey, and stay tuned for more insights and stories from St. Emlyn's. Keep learning, keep teaching, and be the best educator you can be.

Saturday Oct 29, 2016
Ep 82 - Apparent Life Threatening Events in Babies
Saturday Oct 29, 2016
Saturday Oct 29, 2016
Here's the podcast on BRUE and ALTE's in the emergency department.

Wednesday Oct 12, 2016
Ep 81 - Difficult Conversations with Children in Critical Care with Liz Crowe
Wednesday Oct 12, 2016
Wednesday Oct 12, 2016
Helping Children Understand Tragedy: Guidance for Parents and Professionals
In a recent St Emlyn's podcast, Iain Beardsell and Liz Crowe, an advanced social worker in a pediatric intensive care unit in Brisbane, explored the critical topic of how to communicate with children during tragic situations. The discussion emphasized the importance of honesty and directness when dealing with topics like illness, death, and other forms of hardship.
Understanding the Context
Historically, children in many cultures were more regularly exposed to the realities of life, such as birth and death. In contrast, modern Western societies often shield children from these experiences. However, Liz asserts that children are more perceptive and resilient than we give them credit for, and attempts to protect them from all emotional pain can be detrimental. Shielding children from the truth can lead to confusion and increased anxiety, as they often sense when something is wrong, even if it is not explicitly communicated to them.
The Importance of Honesty
When difficult situations arise, such as a family member being diagnosed with a serious illness or being involved in an accident, adults may feel the instinct to protect children by withholding information. However, research and experience show that children cope better when they are informed and involved. Children, especially those under ten, can mistakenly believe they are responsible for negative events due to their egocentric worldview. Therefore, it is crucial to communicate clearly and truthfully, helping them understand the situation without assigning blame to themselves.
Balancing Protection and Reality
Parents naturally want to protect their children from pain. However, overprotection can prevent children from learning to deal with disappointment and hardship, essential components of developing resilience. Liz argues that by being overly protective, we may contribute to rising rates of depression and mental health issues among young people. It's essential to prepare children for life's challenges by allowing them to experience and understand difficult emotions in a supportive environment.
Practical Approaches to Communication
When faced with the need to communicate difficult news to children, it's important to empower familiar adults—such as parents or guardians—to have these conversations rather than leaving them to strangers. Here’s a suggested approach:
- Preparation: Prepare the adults involved in the child's life by discussing the importance of honest communication and the possible impacts of the conversation.
- Setting Expectations: Describe what the child might see, hear, and feel to reduce anxiety and set clear expectations.
- Use Specific Language: Avoid euphemisms. Use specific medical terms like "neuroblastoma" or "head injury" to describe the situation accurately.
- Timing and Environment: Choose an appropriate time and setting for the conversation, avoiding moments when the child might be tired or distracted.
- Stick to the Facts: Provide clear, factual information without overwhelming the child. Keep explanations straightforward and allow time for processing.
- Encourage Questions: Allow the child to ask questions and answer them honestly. It’s okay to admit if you don’t have all the answers.
- Ongoing Support: Be available for follow-up conversations, as children may revisit these topics as they process the information.
Using Accurate Language
It’s crucial to use accurate language when discussing severe issues. Avoid using vague terms like "poorly," which can lead to misunderstandings. For example, describing a child as "very sick" without specifying the illness can cause confusion and fear, especially if the child later associates the term with less severe conditions. Using specific medical terminology helps children differentiate between different types of illnesses and their severity.
Long-Term Impact on Children
Many parents and caregivers worry that exposure to tragedy will permanently damage their children. While such experiences can indeed be life-changing, they do not necessarily result in negative outcomes. Children who experience the death of a sibling or parent may grieve and feel pain, but they can also develop greater empathy and understanding of life's complexities. Research indicates that while children in these situations may have higher levels of anxiety, they are not necessarily less successful academically or socially. They often develop a deeper sensitivity and a better understanding of life.
The Role of Counseling and Support
While counseling can be helpful, Liz cautions against making it the default response. Instead, she suggests that families should be encouraged to navigate these challenges on their own, seeking professional help only if they find themselves unable to cope. This approach fosters resilience and self-reliance, teaching children that while therapy is a valuable resource, it's not always necessary.
Conclusion: Building Resilience
Ultimately, difficult conversations with children about tragedy are a necessary part of life. By approaching these conversations with honesty, clarity, and support, we can help children navigate their emotions and develop the resilience needed for future challenges. Whether as parents or healthcare professionals, our role is to guide children through these experiences, providing the tools and understanding they need to grow and thrive.
At St Emlyn's, we believe that while we can't shield children from all of life's difficulties, we can help them face these challenges with courage. The experiences that children go through, even the painful ones, can serve as opportunities for growth and learning. With the right support, children can emerge from these experiences stronger and better equipped to handle life's complexities. Our goal is to create a safe space for children to express their feelings, ask questions, and ultimately, develop the resilience they need to navigate the ups and downs of life

Monday Oct 03, 2016
Ep 80 - EuSEM Half Time Talk
Monday Oct 03, 2016
Monday Oct 03, 2016
Simon and Iain chat about the first few days at EuSEM in Vienna. Some of the clinical and social highlights. We also have a bonus podcast at the end recorded with a volunteer at Iain's "Podcasting for Beginners'" talk. For more from EuSEM (The European Society for Emergency Medicine) congress follow the #eusem16 hashtag on Twitter.

Thursday Sep 15, 2016
Ep 79 - Critical Appraisal Nugget: Selection Bias
Thursday Sep 15, 2016
Thursday Sep 15, 2016
Summary of Selection Bias in Medical Research
Introduction
Selection bias is a critical issue in medical research that can undermine the validity of study findings. It occurs when there is a systematic difference between the study population and the broader population the research aims to represent. Understanding selection bias is essential for clinicians and researchers, as it can lead to questionable conclusions and affect clinical practice. This summary covers the definition of selection bias, its sources, and ways to mitigate it, along with a case study illustrating its impact.
What is Selection Bias?
Selection bias happens when the participants in a study do not accurately reflect the general population. This discrepancy can result from various factors, including how patients are selected, the setting of the study, and the timing of patient recruitment. Such biases can skew research results, making them less applicable to real-world situations. As medical professionals rely heavily on research to inform clinical decisions, recognizing and addressing selection bias is crucial.
Sources of Selection Bias
-
Study Environment
The environment where a study is conducted can significantly influence patient selection. For instance, patients in a general practitioner's office might have a lower prevalence of serious conditions compared to those in an emergency department. Additionally, studies in specialized tertiary care centers often include patients with more severe or rare conditions, which may not represent the general patient population. This can lead to overestimating or underestimating the effectiveness of treatments or the accuracy of diagnostic tests.
-
Timing of Patient Recruitment
The timing of patient recruitment is another source of selection bias. The stage of illness at which patients are recruited can affect study outcomes, especially in diagnostic studies. For example, the diagnostic value of CRP for appendicitis changes depending on when it is measured. Additionally, certain conditions may present differently depending on the time of day or week, potentially leading to an incomplete understanding of a condition's prevalence or severity if the study only includes patients from specific times.
-
Retrospective vs. Prospective Studies
Retrospective studies, which rely on historical data, are particularly vulnerable to selection bias. These studies may selectively include data from periods with better patient outcomes, leading to skewed results. They may also suffer from incomplete data or changes in diagnostic criteria over time, making it difficult to generalize findings. Prospective studies, while more controlled, also need careful planning to avoid selection bias, especially in defining inclusion and exclusion criteria.
-
Convenience Sampling
Convenience sampling involves selecting patients based on availability rather than a structured protocol, often due to resource limitations. This can result in a non-representative sample, such as including only daytime patients who might differ from those presenting at night. While convenience sampling can be a pragmatic choice, it often leads to underrepresentation of certain patient groups, potentially biasing study findings.
Mitigating Selection Bias
To mitigate selection bias, researchers should strive for comprehensive sampling strategies, such as random or consecutive sampling. Where complete sampling is not possible, they should transparently report potential biases and the measures taken to minimize them. For instance, using screening logs or adjusting for demographic differences can help address disparities between recruited and non-recruited patients. Sensitivity analyses can also be used to understand the impact of excluding certain patient groups.
Case Study: Thrombolysis in PEA Cardiac Arrest
A recent journal club discussion highlighted a retrospective cohort study by Shereefi et al., examining the efficacy of half-dose thrombolysis in patients with PEA cardiac arrest and confirmed pulmonary embolism (PE). The study raised concerns due to several potential biases. The arbitrary selection of a 23-month inclusion period, without a clear rationale, suggests the possibility of survival bias, as it included only patients who survived long enough to receive a confirmatory diagnosis of PE. This selective inclusion means the findings might overestimate the treatment's effectiveness, as the study only considered patients with a relatively favorable prognosis.
Moreover, the study's setting in a specialized environment and the inclusion of only confirmed PE cases limit the generalizability of the results. In practice, thrombolysis may be administered based on clinical suspicion rather than confirmed diagnosis, which involves a broader and potentially more diverse patient group. The study's focus on survivors also excludes those who may have died before a diagnosis, further skewing the data towards more favorable outcomes.
Implications of Selection Bias
Selection bias can significantly impact the interpretation of study results and, consequently, clinical decisions. It can lead to over- or underestimation of a treatment's effectiveness or the prevalence of a condition. This bias can also affect healthcare policy and practice guidelines, potentially disadvantaging underrepresented patient groups. For example, guidelines developed from biased research may fail to address the needs of older adults or those with comorbidities if these groups are underrepresented in studies.
Conclusion
Selection bias is a pervasive issue that can undermine the credibility of medical research. It arises from various sources, including the study environment, timing of recruitment, study design, and sampling methods. While complete elimination of selection bias is challenging, awareness and careful methodological design can mitigate its effects. Researchers and clinicians must critically appraise studies, considering potential biases and their implications for clinical practice. By doing so, we can make more informed decisions and improve patient care. At St. Emlyns, we continue to explore these critical appraisal topics to support evidence-based practice.

Friday Sep 09, 2016
Ep 78 - Intro to EM: Upper GI bleeding
Friday Sep 09, 2016
Friday Sep 09, 2016
Comprehensive Overview of Upper GI Bleeds in Emergency Medicine
Upper gastrointestinal (GI) bleeding is a common and potentially life-threatening condition encountered in emergency medicine. It encompasses a broad spectrum of clinical presentations, ranging from mild cases with minimal blood loss to severe, life-threatening hemorrhages. Understanding the various causes, accurate risk stratification, and appropriate management strategies are crucial for optimizing patient outcomes.
Causes and Mimics of Upper GI Bleeding
Upper GI bleeding originates from the upper part of the gastrointestinal tract, including the esophagus, stomach, and the duodenum. Common causes include:
- Mallory-Weiss Tears: These are tears at the gastroesophageal junction caused by forceful vomiting or retching.
- Gastritis and Peptic Ulcer Disease: These conditions involve inflammation or ulceration in the stomach or duodenum and are frequent causes of bleeding.
- Esophageal Varices: Dilated veins in the esophagus, often due to liver disease and portal hypertension, can rupture and cause severe bleeding.
- Gastroesophageal Reflux Disease (GERD): Chronic acid reflux can lead to esophagitis and bleeding.
It is also important to distinguish true upper GI bleeding from conditions that mimic it. For example, blood from a nosebleed (epistaxis) may be swallowed and later vomited, simulating GI bleeding. Additionally, differentiating between hemoptysis (coughing up blood) and hematemesis (vomiting blood) is essential for accurate diagnosis.
Risk Stratification Using the Glasgow-Blatchford Score (GBS)
Effective management of upper GI bleeding begins with risk stratification to determine the severity of the condition and the need for urgent intervention. The Glasgow-Blatchford Score (GBS) is a widely utilized tool that helps predict the need for medical treatment and the risk of adverse outcomes. It considers several clinical parameters, including:
- Blood Urea Nitrogen (BUN): Elevated levels suggest significant bleeding.
- Hemoglobin Levels: Low levels indicate blood loss.
- Systolic Blood Pressure: Hypotension is a sign of significant hemorrhage.
- Pulse Rate: Tachycardia can indicate a compensatory response to blood loss.
- Clinical Signs: The presence of melena, syncope, or liver disease increases the risk score.
Patients with a GBS of zero are considered low risk and may be suitable for outpatient management with appropriate follow-up. Those with higher scores require hospitalization for further evaluation and treatment, including possible endoscopy.
Initial Management and Resuscitation
The immediate management of patients with upper GI bleeding involves stabilizing the patient and preventing further complications. Key steps include:
- Airway Management: Ensuring a clear and secure airway is critical, particularly in patients with altered consciousness or ongoing vomiting.
- Fluid Resuscitation: Intravenous fluids are administered to maintain hemodynamic stability.
- Blood Product Transfusion: In cases of significant bleeding, transfusions of packed red blood cells, fresh frozen plasma, and platelets may be necessary to manage blood loss and correct coagulopathies.
Role of Endoscopy
Endoscopy is a crucial diagnostic and therapeutic tool in managing upper GI bleeding. It should ideally be performed within 24 hours of presentation to determine the source of bleeding and provide treatment. Urgent endoscopy is particularly indicated for patients with hemodynamic instability or signs of significant bleeding.
Special Considerations for Variceal Bleeding
Variceal bleeding, often seen in patients with chronic liver disease, requires specific management strategies due to its severity and associated complications. Key considerations include:
- Terlipressin: A vasoconstrictor that helps reduce portal pressure and control bleeding in variceal cases.
- Antibiotic Prophylaxis: Administered to prevent infections, which are common in patients with liver disease and variceal bleeding.
- Balloon Tamponade: In situations where endoscopy is not immediately available, a Sengstaken-Blakemore tube can be used as a temporary measure to control bleeding. This procedure should be performed with caution and preferably under the supervision of an experienced specialist.
Multidisciplinary Approach
The management of upper GI bleeding, particularly severe cases, requires a coordinated approach involving multiple specialties. The emergency physician plays a central role in initial stabilization and diagnosis, but collaboration with gastroenterologists, anesthetists, hematologists, and critical care teams is essential. This multidisciplinary team ensures comprehensive care, from initial resuscitation and endoscopic intervention to ongoing monitoring and treatment in critical care settings.
Disposition and Follow-Up
The decision to admit or discharge a patient with upper GI bleeding depends on the severity of the bleeding, patient stability, and the results of risk stratification. Low-risk patients (GBS of zero) may be discharged with a plan for outpatient follow-up and endoscopy. In contrast, patients with higher risk scores or ongoing symptoms should be admitted for further evaluation and treatment.
Conclusion
Upper GI bleeding is a critical condition that demands prompt recognition, accurate assessment, and effective management. By utilizing risk stratification tools like the Glasgow-Blatchford Score and employing a multidisciplinary approach, healthcare providers can significantly improve patient outcomes. Proper diagnosis and timely intervention, including endoscopy and appropriate supportive care, are vital components of successful management.
As always, we encourage healthcare professionals to share their experiences and best practices in managing upper GI bleeds. Engage with us on social media or leave a comment on this blog post to contribute to the ongoing discussion on improving emergency medicine care.

Wednesday Aug 24, 2016
Ep 77 - Critical Appraisal Nugget 2: Blinding and Masking in clinical trials
Wednesday Aug 24, 2016
Wednesday Aug 24, 2016
Understanding Blinding in Clinical Trials: A Comprehensive Guide
Blinding, also referred to as masking, is a crucial methodological approach used in clinical trials to eliminate bias and ensure the validity of study outcomes. This practice involves keeping study participants, clinicians, and researchers unaware of the treatment assignments. The goal is to prevent the knowledge of treatment allocation from influencing behaviors, perceptions, or evaluations, thus maintaining the integrity of the research.
Types of Blinding in Clinical Trials
Single Blinding: In this approach, only the participants are unaware of the treatment they receive. For example, in a drug trial comparing an anticoagulant to a placebo, participants do not know which they are receiving. This method helps prevent the placebo effect or other biases arising from participants' expectations. Ensuring effective single blinding requires that the placebo and active treatment appear identical in all sensory aspects, including appearance, taste, and even side effects.
Double Blinding: This method extends the concealment to both participants and the clinicians or researchers administering the treatment. It is crucial because knowledge of the treatment can influence the clinical management of the patient or the interpretation of symptoms. For example, if a doctor knows a patient is receiving a placebo, they might provide less attentive care. Double blinding helps ensure that all patients receive consistent care, and it prevents clinicians from unintentionally influencing the outcomes based on their expectations.
Triple Blinding: The most comprehensive form of blinding, triple blinding, includes blinding the data analysts as well. This method prevents bias during the interpretation of study results, as analysts are unaware of which group received the treatment. This approach is particularly important when the data analysis involves subjective judgments or when the analysis plan is not strictly predefined. Triple blinding helps ensure that data is handled objectively, leading to more reliable conclusions.
Importance of Blinding in Clinical Trials
Blinding is essential to minimize various forms of bias that can compromise the validity of clinical trials. These biases include:
-
Participant Bias: When participants know the treatment they are receiving, it can influence their reporting of symptoms and outcomes, skewing the study results.
-
Observer Bias: Clinicians and researchers may consciously or unconsciously alter their assessments based on their knowledge of the treatment allocation. This can affect how symptoms are recorded or how interventions are implemented, potentially leading to biased outcomes.
-
Analyst Bias: Data analysts may be influenced by their expectations or hypotheses if they know which treatment group participants belong to. This can affect the objectivity of the data analysis, making the results less reliable.
Practical Challenges in Blinding
Despite its importance, blinding is not always feasible or ethical in all types of studies. For example, in trials comparing physical interventions like a wrist splint versus a plaster cast, it is impossible to blind participants or clinicians due to the visible nature of the treatments. In such cases, researchers must adopt a pragmatic approach, using rigorous randomization and transparent reporting to mitigate potential biases.
A notable case highlighting the challenges of blinding is a study conducted by Dan Horner and colleagues on the treatment of calf deep vein thrombosis (DVT). The study compared the use of warfarin with no anticoagulation. Ideally, the study would have included a placebo group, but ethical and practical concerns made this impossible. Patients on warfarin require regular monitoring and dose adjustments, which could not ethically be simulated for a placebo group. As a result, the study was conducted without blinding but still provided valuable insights into the treatment's potential benefits.
Sham Interventions in Blinding
In some studies, particularly those involving surgical procedures, sham interventions are used to maintain blinding. This involves performing procedures on the control group that mimic the intervention without providing therapeutic benefits. For instance, in trials assessing surgical techniques, control group participants might undergo anesthesia and incision without actual surgery. This method is ethically sensitive but can be crucial in preventing bias from influencing the study's outcomes.
Blinding in Diagnostic Studies
Blinding is also vital in diagnostic studies, where it ensures that the assessment of diagnostic tests is not influenced by pre-existing knowledge about the patients. For instance, in evaluating a new diagnostic test like a D-dimer test for pulmonary embolism, blinding the interpreters of test results is essential. It prevents bias in the interpretation of test outcomes, ensuring that results are evaluated based on the test's performance rather than expectations or assumptions.
Conclusion
Blinding is a fundamental component of clinical trial design, crucial for minimizing bias and ensuring the validity of study findings. Whether it is single, double, or triple blinding, the technique helps maintain objectivity in clinical research, making the results more reliable and trustworthy. While blinding is not always possible, especially in trials involving visible interventions, researchers must strive to minimize bias through careful study design and transparent reporting.
As readers and critical appraisers of clinical research, it is essential to look for evidence of blinding and consider its impact on the validity of study results. Understanding the importance and challenges of blinding can help us better interpret clinical trial outcomes and make informed decisions in healthcare.
Thank you for joining us at St. Emlyn's. Stay curious, critically appraise the evidence, and continue exploring the fascinating world of clinical trials. Until next time, stay informed and engaged in advancing medical knowledge.

Wednesday Aug 17, 2016
Ep 76 - Communication workshop with Liz Crowe (SMACC DUB)
Wednesday Aug 17, 2016
Wednesday Aug 17, 2016
Optimizing Communication in Healthcare: Key Takeaways from the SMACC Conference
At the recent SMACC conference in Dublin, a notable workshop led by Liz Crowe and Steve Philpott focused on enhancing communication skills in healthcare. This workshop emphasized the importance of understanding one's own communication style and how it impacts interactions with patients, colleagues, and even personal relationships.
Understanding Communication Styles
The workshop began by highlighting that communication is influenced by personality traits, which shape how we express and receive information. One key distinction is between extroverts and introverts. Extroverts often gain energy from social interactions and tend to speak quickly, sharing ideas readily. In contrast, introverts recharge through solitude and may take longer to articulate their thoughts. Recognizing these traits is crucial in healthcare settings, where both types bring valuable strengths to a team. For instance, extroverts may lead discussions and drive actions, while introverts often provide thoughtful insights after careful consideration.
Balancing Team Dynamics
A critical takeaway was the importance of having a balanced mix of personality types within a team. A group dominated by extroverts might lack depth in decision-making, while a team of introverts might struggle with timely execution. Effective teams combine these traits, ensuring diverse perspectives and approaches. For example, when tackling tasks like developing protocols or organizing events, having both meticulous "get it right" individuals and efficient "get it done" members ensures thorough and timely outcomes.
Practical Communication Strategies
The workshop provided several practical strategies to improve communication:
1. Signposting
Signposting involves clearly highlighting key points throughout a conversation, ensuring they are understood and remembered. In healthcare, this technique is essential for communicating critical information, such as diagnoses or treatment plans. By repeatedly emphasizing important messages, healthcare professionals can help patients and families grasp complex information more effectively.
2. Avoiding "But"
A simple yet powerful language adjustment discussed was avoiding the word "but." Using "but" can negate the positive aspects of a statement, creating a dismissive tone. Instead, substituting "but" with "and" maintains a constructive dialogue. For example, saying, "You did a great job, and improving your time management will make you even more effective," keeps the conversation positive and forward-looking.
3. First and Last Impressions
The first and last things said in a conversation are often the most memorable, especially in stressful situations. Setting a serious tone at the beginning of a difficult conversation and summarizing key points at the end ensures that the main messages are clear. This approach is crucial when delivering bad news or discussing sensitive topics, as it helps manage expectations and emotions.
4. Chunking Information and Allowing Pauses
Breaking down complex information into smaller, manageable chunks and allowing pauses helps listeners process and understand better. This technique is particularly useful when communicating with patients and families who may be overwhelmed with medical jargon and stress. Pauses give them time to absorb the information and ask questions, demonstrating empathy and patience.
Handling Difficult Conversations
Discussing sensitive topics, such as poor prognosis or end-of-life care, requires a careful balance of empathy and honesty. The workshop emphasized acknowledging optimism bias—the tendency to hold onto hope even when the prognosis is poor. Healthcare professionals should acknowledge the family's hope while gently grounding them in reality. For example, expressing understanding of their hopes while clearly stating the medical expectations helps families navigate difficult emotions.
The Platinum Rule
The platinum rule, which goes beyond treating others as you would like to be treated, focuses on treating others as they would like to be treated. This involves understanding the communication preferences of patients and families. Some may prefer detailed explanations, while others might want a broader overview. Asking about their preferences and tailoring the communication accordingly enhances their sense of control and satisfaction.
Staying Connected
Maintaining a connection with patients and families is crucial, especially in challenging situations. While outcomes may not always be within control, the process of communication is. Ensuring that patients and their families feel heard, respected, and supported can make a significant difference in their healthcare experience. This connection is not just about delivering information but also about showing empathy and understanding.
Conclusion
The SMACC conference workshop provided invaluable insights into improving communication in healthcare. By understanding our own communication styles, appreciating the strengths of different personality types, and employing practical strategies like signposting, avoiding "but," and using the platinum rule, healthcare professionals can enhance their interactions with patients and colleagues. Effective communication is not just about conveying information; it's about building trust, understanding, and a positive work environment.
These skills are essential for providing high-quality patient care and fostering a supportive workplace culture. The workshop highlighted that good communication can prevent misunderstandings, reduce the likelihood of complaints, and ultimately save time. By investing a few extra minutes in effective communication, healthcare professionals can significantly improve patient outcomes and satisfaction.
In summary, the key to effective communication in healthcare lies in understanding ourselves and others, being clear and empathetic, and continuously refining our skills. Whether in patient interactions or team collaborations, these principles help create a more compassionate and efficient healthcare environment.

Wednesday Aug 10, 2016
Ep 75 - Critical Appraisal Nugget 1: Randomisation
Wednesday Aug 10, 2016
Wednesday Aug 10, 2016
Understanding Randomization in Clinical Trials: A Guide for Critical Appraisal
Welcome to the St. Emlyn's blog, your go-to resource for insights into emergency medicine and critical care. Today, we're diving into a crucial aspect of clinical research: randomization. Whether you're preparing for exams like the FR-KEM or just want to deepen your understanding of clinical trials, understanding randomization is key to critical appraisal. This blog post will walk you through the essentials, common pitfalls, and best practices for ensuring robust study design.
What is Randomization?
Randomization is a foundational process in clinical trials, particularly those evaluating interventions. It refers to the random allocation of participants into different treatment groups. This process aims to eliminate selection bias and ensure that differences in outcomes can be attributed to the intervention itself rather than other factors.
Why is Randomization Important?
Randomization is crucial because it helps establish causality. Without it, studies might only reveal associations rather than true cause-and-effect relationships. For example, if we observe patients receiving different treatments in a non-randomized manner, systematic differences between the groups—such as varying standards of care—could confound the results. Randomization seeks to balance these factors, allowing for a clearer interpretation of the intervention's effectiveness.
Key Components of Randomization
-
Random Allocation: This is the process of assigning participants to treatment groups purely by chance. It can be done using random number tables, computer-generated sequences, or other methods that ensure allocation is not influenced by investigators or participants.
-
Allocation Concealment: This involves hiding the allocation sequence from those involved in enrolling participants. It's vital to prevent selection bias, where researchers might consciously or unconsciously influence the assignment of participants to specific groups.
-
Blinding: While not a part of randomization per se, blinding is closely related. It refers to keeping participants, healthcare providers, and researchers unaware of which treatment group participants are in. This prevents performance and detection biases.
Common Pitfalls in Randomization
Despite its importance, randomization can be implemented poorly, leading to biased results. Here are some common pitfalls:
-
Inadequate Randomization Methods: Methods like assigning treatments based on birth dates or day of the week might seem random but can introduce systematic biases. For instance, there could be differences in care based on the day or time, making these methods unreliable.
-
Failure to Conceal Allocation: In the past, brown envelope methods were used, where the treatment assignment was sealed in an envelope. However, this method is vulnerable to tampering. For instance, researchers might be tempted to "peek" at the assignment and selectively enroll participants, compromising the study's integrity.
-
Small Sample Sizes: Small trials are particularly vulnerable to imbalance in baseline characteristics between groups purely by chance. This can lead to skewed results that do not accurately reflect the intervention's efficacy.
Best Practices in Randomization
To ensure robust and reliable results, certain best practices should be followed:
-
Use of Reliable Randomization Methods: In modern trials, computer-generated random numbers are the gold standard. They provide true randomness and can be tailored to the specific needs of the study.
-
Allocation Concealment Techniques: More sophisticated methods like centralized randomization, where a third party manages the allocation process, can help maintain concealment. In some studies, web-based or voice-based systems are used, which provide real-time allocation while preventing researchers from manipulating the process.
-
Stratification and Block Randomization: To address the issue of unequal distribution of participants' characteristics, stratification and block randomization are employed. Stratification involves grouping participants based on certain characteristics (e.g., disease severity) and ensuring even distribution across treatment groups. Block randomization, on the other hand, ensures that each treatment group has an equal number of participants within defined blocks, maintaining balance throughout the study.
The Role of Randomization in Analyzing Results
When analyzing the results of a randomized controlled trial (RCT), the first step is to examine the baseline characteristics of the treatment groups. This is often presented in Table 1 of a study. The purpose is to ensure that randomization has successfully created comparable groups. If significant differences exist, they could confound the results, making it harder to attribute outcomes to the intervention alone.
Another critical aspect is to consider the size of the trial. Larger studies are generally better at balancing characteristics between groups, reducing the likelihood of chance imbalances. However, even in well-randomized studies, it's possible for imbalances to occur, especially in smaller trials. Researchers must acknowledge these potential imbalances and adjust their analyses accordingly.
Practical Considerations in Emergency Medicine
In emergency medicine, the need for rapid, reliable randomization methods is particularly pressing. Web-based randomization systems offer a convenient solution, providing quick, secure, and tamper-proof allocation. Similarly, voice-based systems, where a computer assigns treatment groups via a phone call, are another practical option.
For those conducting smaller trials, there are accessible tools available, such as Sealed Envelope (sealedenvelope.com), which offers randomization services tailored to smaller studies. These tools help maintain the integrity of the randomization process, even in resource-limited settings.
Special Considerations: Trials with Diverse Populations
In clinical trials, particularly in emergency settings, researchers often encounter a wide range of patient severities. For instance, in head injury studies, patients can vary significantly in their Glasgow Coma Scale (GCS) scores. In such cases, simple randomization may inadvertently group all severe cases into one treatment arm, skewing the results.
To mitigate this, researchers use stratification, ensuring that key subgroups (e.g., GCS < 8) are evenly represented across treatment groups. This not only improves the internal validity of the study but also enhances the power of the statistical analyses, providing more reliable results.
Advanced Randomization Techniques
As trials become more complex, so do the randomization techniques. Block randomization is one such method that ensures each treatment group receives participants throughout the study, rather than in uneven waves. For example, rather than having all participants receive treatment A first, followed by treatment B, block randomization allocates treatments in smaller blocks (e.g., groups of 20), maintaining balance throughout.
This method is particularly valuable in trials with interim analyses or those that may stop early due to significant findings. It ensures that at any given point, the distribution of participants is roughly equal, allowing for fair and accurate assessment of the treatment effects.
Conclusion: The Importance of Rigorous Randomization
Randomization is the cornerstone of robust clinical trial design. It minimizes biases, balances baseline characteristics, and supports the validity of causal inferences. However, the process must be meticulously planned and executed. From choosing the right method to ensuring allocation concealment, every step is crucial in maintaining the integrity of the study.
For clinicians and researchers, understanding the nuances of randomization helps in critically appraising literature and designing their own studies. Whether you're preparing for an exam or conducting a trial, appreciating the intricacies of randomization will enhance your ability to interpret and apply clinical research findings effectively.
At St. Emlyn's, we emphasize the importance of thorough critical appraisal skills. By mastering these concepts, you'll be better equipped to discern high-quality evidence and make informed decisions in your clinical practice. Stay tuned for more insights and practical tips on navigating the world of clinical research.
Sunday Jul 31, 2016
Sunday Jul 31, 2016
Effective Trauma Handovers: Best Practices and Key Considerations
Trauma handovers are critical transitions in patient care, transferring responsibility from pre-hospital teams to in-hospital teams. These moments are crucial for ensuring patient safety and the continuation of effective treatment. This summary explores the best practices for trauma handovers, focusing on preparation, timing, communication, and the integration of feedback.
Preparation: Utilizing Golden Time
Effective trauma handovers begin with thorough preparation. The period between receiving the notification of an incoming trauma patient and their arrival is often called "golden time." This time should be used to organize and prepare the multidisciplinary team, including in-patient specialists, ED staff, nurses, doctors, and radiologists. Key preparatory steps include:
- Role Allocation: Assign clear responsibilities, such as the trauma team leader, scribe, airway manager, and primary survey conductor. It is crucial to ensure that team members are both competent and confident in their assigned roles, as these attributes, while related, are distinct.
- Predictive Planning: Use pre-hospital information to anticipate the patient's needs. For instance, a report of a patient with a chest stab wound and hypotension suggests the need to prepare for a thoracotomy.
Timing and Coordination
Timing is essential in trauma care, particularly in avoiding early calls to the trauma team. At Southampton, the recommended practice is to call the team together approximately 15 minutes before the patient’s expected arrival, avoiding exact time estimates. This strategy helps maintain team readiness and focus. The risks of early calls include loss of focus due to prolonged waiting and the potential for team members to become distracted by other tasks.
Conducting the Team Briefing
A comprehensive and unified briefing is vital upon the trauma team’s assembly. This briefing should involve the entire multidisciplinary team, preventing any division into subgroups and ensuring that all members receive the same information. A good practice is for team members to introduce themselves using first names, which helps break down hierarchical barriers and fosters a collaborative environment. The briefing should also include a mission rehearsal, outlining the specific tasks and roles each member will perform upon the patient's arrival.
The Handover Process
The actual handover begins when the patient arrives. The in-hospital team leader should introduce themselves to the pre-hospital team and determine if the patient is stable enough for a hands-off handover. This approach, modeled after military practices, ensures that the handover is conducted calmly and clearly. If the patient is unstable, the pre-hospital team should continue leading the resuscitation until it is safe to hand over control.
A structured framework, such as AppMist (Age, Time of injury, Mechanism, Injuries, Signs, and Treatments), should be used to deliver concise and critical information during the handover. This approach ensures that only the essential information is communicated, focusing on the most pertinent details for the ongoing treatment.
Addressing Pre-Hospital Challenges
The pre-hospital environment is inherently stressful and challenging, with limited resources and a high cognitive load. Pre-hospital teams often face the dual pressures of managing critically ill patients and communicating effectively with the receiving hospital. It is crucial for in-hospital teams to recognize these challenges and refrain from criticizing or undermining pre-hospital efforts during the handover. Instead, the focus should be on receiving and clarifying the necessary information to continue patient care.
Pre-hospital teams should aim to deliver concise, relevant information during the handover. Ending the handover with a clear statement, such as "That completes my handover," followed by an offer to answer any urgent questions, helps ensure clarity and completeness.
Feedback and Continuous Improvement
Closing the feedback loop is an essential aspect of improving trauma care. Providing feedback to pre-hospital teams about patient outcomes helps refine their assessment and treatment strategies. This feedback should be delivered sensitively, acknowledging the emotional and high-pressure nature of pre-hospital work.
Constructive feedback should focus on confirming or refuting pre-hospital assessments and decisions, providing a learning opportunity for future cases. It is essential to approach feedback with empathy and professionalism, fostering a supportive environment for continuous improvement.
Controversial Aspects and Best Practices
Calling the Full Trauma Team: There is a debate over whether to always call the entire trauma team for every alert. At our hospital, we favor over-calling to ensure that all necessary resources are immediately available, even if it means releasing some staff after assessing the situation.
Pre-Hospital Requests for Specific Interventions: In-hospital teams must use their discretion when responding to pre-hospital requests for specific interventions or specialist involvement. Trust and familiarity with the pre-hospital team's capabilities influence these decisions. For example, while cardiothoracic surgeons are not standard members of our trauma team, they may be involved in cases of traumatic cardiac arrest with penetrating trauma.
Conclusion: A Framework for Effective Trauma Handover
Effective trauma handovers are essential for patient safety and optimal care. This process requires careful preparation, clear communication, and seamless coordination between pre-hospital and in-hospital teams. By adhering to standardized practices, fostering a collaborative environment, and integrating constructive feedback, healthcare providers can significantly enhance the quality of trauma care.
We encourage healthcare professionals to share their experiences and insights, contributing to a broader understanding of best practices in trauma handovers. Whether you are working in trauma centers, units, or in different healthcare systems worldwide, your input is invaluable in refining these critical processes.
Thank you for engaging with this discussion on the St Emlyns blog. We look forward to continuing this conversation and exploring ways to improve patient care in emergency medicine.

Friday Jul 08, 2016
Friday Jul 08, 2016
Enhancing Pre-Hospital to Hospital Handover: Insights from SMACC Dublin
The SMACC Dublin conference provided a valuable platform for discussing the crucial handover process from pre-hospital teams to hospital staff. This transition is essential for patient safety and continuity of care, as it involves conveying critical information from emergency responders to hospital-based healthcare professionals. The discussion at the conference highlighted several key issues, best practices, and strategies to improve this critical interface.
The Emotional Landscape and Communication Challenges
Dr. Natalie May, reflecting on her shift from hospital to pre-hospital care, emphasized the emotional challenges and the need for empathy and understanding between both teams. Pre-hospital providers often face a tense environment upon hospital arrival, with varying degrees of reception from the hospital team. This tension can arise from perceived disrespect or a lack of understanding of the pre-hospital team's challenges, which can complicate the handover process.
A significant issue in handover is the lack of structured communication. The fast-paced environment of the emergency department (ED) can pressure pre-hospital providers to quickly pass on patients and information, sometimes resulting in incomplete or rushed handovers. To address this, the use of structured communication tools like the AD MISSED acronym (Age, Date/Time, Mechanism of Injury, Injuries, Signs/Symptoms, Treatments, and Decisions) was recommended. This structure helps ensure that all essential information is conveyed systematically, minimizing the risk of information loss.
Best Practices for Handover
One highlighted best practice is the implementation of a clear and consistent protocol. For instance, a Texas hospital has adopted a "hands-off" period during handover, where the receiving team does not intervene until the pre-hospital team has completed their report. This approach helps maintain focus on the verbal communication of critical details without distractions, ensuring a comprehensive transfer of information.
The role of the trauma team leader is also critical. They act as the primary point of contact, receiving the handover and ensuring that all relevant team members understand the conveyed information. The trauma team leader is responsible for verifying the accuracy of the information, clarifying any uncertainties, and coordinating subsequent actions. This leadership role is crucial in maintaining a smooth and efficient handover process.
Overcoming Communication Barriers
Differences in communication styles and preferences between hospitals can pose challenges. The discussion emphasized the need for pre-hospital teams to be adaptable, potentially rehearsing handovers and using aids like whiteboards. Regular joint training sessions between pre-hospital and hospital teams were recommended to align expectations and familiarize each side with the other's protocols. The use of digital tools, such as secure messaging apps, can also facilitate better communication and continuity of care.
The physical environment during handover significantly impacts its effectiveness. A calm, organized setting with minimal interruptions is ideal for ensuring a thorough transfer of information. Designating a specific area for handovers and equipping it with necessary tools, such as a whiteboard and a scribe, can improve the clarity and accuracy of the communication.
The Importance of Feedback
Immediate feedback after handover is crucial for continuous improvement. It allows pre-hospital providers to understand the outcomes of their interventions and the patient's progression. This real-time feedback can highlight areas for protocol refinement and training. Additionally, formal long-term feedback mechanisms, such as follow-up meetings or debriefings, are vital for providing a complete picture of the patient's journey, helping both pre-hospital and hospital teams improve their practices.
Building a Culture of Respect and Understanding
A successful handover process is built on mutual respect and understanding between pre-hospital and hospital teams. Acknowledging the expertise and challenges faced by each group fosters a more cooperative and supportive environment. This respect is essential for enhancing patient care and ensuring a smooth transition from one care setting to another.
To build this culture of respect, regular interdisciplinary workshops and social events can help break down barriers and build rapport among healthcare professionals. Recognizing the unique pressures and responsibilities of each team member contributes to a more harmonious and effective handover process.
Conclusion: Towards a Seamless Continuum of Care
The discussions at SMACC Dublin underscored the importance of an effective handover in emergency medicine. By adopting structured communication protocols, ensuring clear leadership, and fostering a culture of continuous feedback and mutual respect, the gap between pre-hospital and hospital care can be bridged. The ultimate goal is to create a seamless continuum of care, where the transition between healthcare teams is smooth, efficient, and centered on the patient's best interests.
This integrated approach not only improves patient outcomes but also enhances job satisfaction among healthcare providers by reducing miscommunications and misunderstandings. The handover process is a critical component of patient care that requires ongoing attention and improvement.
In conclusion, effective handover practices are essential for ensuring patient safety and continuity of care. The insights from SMACC Dublin provide valuable guidance on refining these practices. By fostering a culture of learning, respect, and collaboration, healthcare providers can ensure that every patient transition is handled with the utmost professionalism and care.

Sunday Jun 26, 2016
Ep 72 - Wellbeing with Liz Crowe
Sunday Jun 26, 2016
Sunday Jun 26, 2016
Prioritizing Personal Well-being in Healthcare: A Guide for Medical Professionals
Introduction
In the healthcare profession, we often prioritize patient care over our own well-being. However, maintaining personal health is crucial for providing high-quality care. This blog post explores the importance of well-being for healthcare professionals and offers practical strategies to enhance it. Given the high risks of burnout and compassion fatigue in our field, understanding and improving our well-being is essential.
The Multi-faceted Nature of Well-being
Well-being encompasses physical health, mental and emotional stability, and social connections. These aspects are vital for maintaining overall health but are often neglected due to the demanding nature of healthcare work. Common practices like relying on caffeine, sugar, and alcohol provide temporary relief but are unsustainable in the long run.
-
Diet and Nutrition
A balanced diet is fundamental to well-being. Many healthcare professionals struggle with poor dietary habits due to busy schedules, often resorting to fast food or skipping meals. This can lead to energy crashes and dependency on unhealthy snacks. Incorporating a balanced diet rich in proteins, fruits, and vegetables can provide sustained energy and support overall health. Simple changes, such as meal prepping and choosing healthy snacks, can significantly improve dietary habits. -
Physical Activity
Regular exercise is essential for physical and mental well-being. Despite busy schedules, finding time for physical activity is crucial. Exercise reduces stress and anxiety, improves mood, and boosts overall health. Simple activities like walking, home workouts, or gym visits can be easily integrated into daily routines, even in small amounts. -
Mental and Emotional Health
The mental and emotional demands of healthcare work are substantial, often leading to stress and burnout. It is essential to prioritize mental health through practices like mindfulness, therapy, or engaging in hobbies. These activities can provide a mental break and improve emotional resilience, helping professionals cope with the pressures of their work environment.
Practical Strategies for Enhancing Well-being
-
Optimizing Diet
Start by reassessing your eating habits. Prepare nutritious meals that are easy to take to work, like sandwiches with whole grains, lean proteins, and vegetables. Keep healthy snacks available, such as fruits and nuts, to avoid reaching for unhealthy options. Hydration is also key; drink plenty of water throughout the day to maintain energy levels and reduce cravings. -
Reducing Caffeine and Sugar
While caffeine and sugar can provide quick energy, they often lead to dependency and health issues. Gradually reduce caffeine intake by substituting with herbal teas or decaf options. Replace sugary snacks with healthier alternatives, and stay hydrated to help manage cravings and maintain energy levels. -
Incorporating Exercise
Integrate physical activity into your routine, starting with realistic goals. Whether it’s a short walk, a quick home workout, or regular gym sessions, exercise is crucial for maintaining health. Even minimal physical activity can have significant benefits, such as improved mood and energy levels. -
Strengthening Social Connections
Social interactions are important for emotional support and well-being. Sharing breaks with colleagues, even with healthier beverage options, can maintain the social ritual and foster community. Building strong relationships with colleagues provides a support network for sharing challenges and celebrating successes. -
Prioritizing Mental Health
Many organizations offer employee assistance programs, including counseling services. Utilizing these resources can help manage stress and other mental health issues. Practices like mindfulness, journaling, or engaging in creative activities can also aid in managing stress and improving mental clarity.
The Role of Sleep
Sleep is critical for maintaining well-being, especially for those working long hours or night shifts. Developing good sleep hygiene is essential, including consistent sleep patterns and a restful sleep environment. Avoiding stimulants like caffeine before bed can also improve sleep quality, which in turn enhances cognitive function and emotional regulation.
Overcoming Barriers to Well-being
-
Time Constraints
Lack of time is a common barrier to maintaining well-being. However, small, consistent changes can make a big difference. Meal prepping, scheduling exercise, and setting aside time for mindfulness are all practical strategies that can fit into a busy schedule. -
Mindset Shifts
It's important to move away from an all-or-nothing mentality. Focus on gradual, sustainable changes rather than attempting to overhaul your entire lifestyle at once. Start with small, manageable goals and adjust them as you progress. -
Seeking Support
A support network is invaluable for maintaining well-being. Whether it’s through friends, family, or professional counselors, sharing your journey can provide motivation and accountability. Colleagues can also offer support and understanding, given the unique challenges of the healthcare profession.
Long-term Benefits
Prioritizing well-being offers numerous benefits, including enhanced capacity for compassionate care, reduced risk of burnout, and a healthier work-life balance. Modeling healthy behaviors can also positively influence colleagues and patients, fostering a culture of well-being within the workplace.
Developing a Personal Well-being Plan
Creating a personal well-being plan involves setting realistic goals and making gradual changes. Assess your current habits and identify areas for improvement. Incorporate elements of physical activity, healthy eating, mental and emotional health, and social connections into your plan. Track your progress, celebrate small victories, and adjust your plan as needed.
Conclusion
As healthcare professionals, taking care of ourselves is crucial to providing the best care for our patients. By prioritizing personal well-being, we can enhance our physical and mental health, improve our capacity for compassionate care, and enjoy a more fulfilling career. Start by making small changes today and share your journey with us at St. Emlyn's. Remember, a healthier you means better care for your patients.

Wednesday Jun 22, 2016
Ep - 71 SMACC Dublin Day 3 Round Up
Wednesday Jun 22, 2016
Wednesday Jun 22, 2016
SMACC Dublin 2023: Key Highlights and Reflections
The SMACC (Social Media and Critical Care) conference is a premier event in the field of critical care and emergency medicine. Held in Dublin, this year’s conference brought together healthcare professionals from around the world to share knowledge, foster connections, and inspire each other. The St Emlyn’s team was in attendance, and we are excited to share our reflections on the final day’s events and the broader impact of the conference.
A Night of Celebration: The SMACC Gala Dinner
The SMACC gala dinner is always a highlight of the conference, and this year was no exception. The event spanned six floors, each offering unique entertainment, from folk music to live bands and a DJ. The atmosphere was electric, filled with opportunities for networking and forging new friendships. The gala dinner epitomizes the community spirit of SMACC, where connections are made not just over discussions of clinical topics but also through shared moments of celebration and joy.
Powerful Plenary Sessions: Stories of Resilience and Compassion
Thursday morning’s plenary session featured four outstanding speakers, each offering a unique perspective on critical care. Kath Maiden opened the session with a moving account of her work in Africa, highlighting the challenges and humbling experiences of providing care in resource-limited settings. Her talk set the tone for a morning of deep reflection on the global disparities in healthcare.
Dr. Nikki Blackwell followed with an impactful presentation on her experiences in disaster zones. She shared stories of repairing ventilators with a Swiss Army knife and managing the emotional strain of working in high-stress environments. Nikki’s talk underscored the resilience required in such settings and the importance of mental health support for healthcare workers.
Ashley Shreves then tackled the crucial topic of palliative care, emphasizing its importance in critical care settings. With an aging population, the need for compassionate end-of-life care is increasingly significant. Ashley urged all healthcare providers to engage in palliative care discussions, making it clear that this responsibility should not be left solely to specialists.
Ashley Liebig’s presentation on the emotional toll of pediatric loss brought a sobering perspective to the day. She recounted her experience as a HEMS nurse dealing with the death of a child, highlighting the complexities of interprofessional communication and the emotional aftermath. Her talk emphasized the need for compassion and support within healthcare teams, particularly after traumatic events.
Promoting Gender Diversity and Leadership
The prominence of female speakers in the plenary session was a notable feature of this year’s SMACC conference. The event has made significant strides in promoting gender diversity, ensuring that expert female voices are heard. This inclusion not only enriches the conference content but also reflects a commitment to fostering a more inclusive and representative community in critical care and emergency medicine.
Navigating the Concurrent Sessions
The concurrent sessions offered a wide array of topics, making it challenging to choose which ones to attend. Tom Evans’ talk on the parallels between training as an Olympian and striving for excellence in medical practice was particularly inspiring. He emphasized the importance of mentorship and structured training in achieving clinical excellence.
Adrian Plunkett’s presentation on "Learning from Excellence" stood out as a refreshing perspective on quality improvement in healthcare. He advocated for the recognition of positive events in clinical practice, arguing that celebrating successes can foster a supportive and constructive work environment. This approach not only improves morale but also encourages continuous learning and improvement.
The Unique Contribution of Peter Brindley
Peter Brindley provided a humorous yet insightful take on teamwork and burnout. His engaging style made complex topics accessible and entertaining. Peter’s emphasis on the importance of maintaining a healthy work-life balance resonated with many attendees, highlighting the need for self-care in high-pressure medical environments.
A Light-Hearted Finale
The conference concluded with a light-hearted finale featuring a competition between the Northern and Southern Hemispheres. This engaging and humorous session provided a fun and relaxed end to the conference, contrasting with the previous year’s more somber conclusion. The finale underscored the importance of taking risks and trying new things, a key theme that ran throughout the conference.
Key Takeaways and Looking Ahead
Reflecting on SMACC Dublin 2023, several key themes emerged. The conference showcased the exceptional quality of education and the value of sharing diverse perspectives. It also highlighted the importance of community, reminding us that we are part of a global network of professionals dedicated to improving patient care. The connections made and lessons learned at SMACC are invaluable, offering new insights and strategies to bring back to our daily practice.
As we look forward to SMACC Berlin 2024, we are excited and anticipating. The conference promises another opportunity to learn, connect, and be inspired. For those unable to attend in person, the wealth of content available through SMACC’s online platforms ensures that the knowledge and spirit of the event can reach a global audience.
In conclusion, SMACC Dublin 2023 was a celebration of excellence in critical care and emergency medicine. It challenged us to think differently, embrace new ideas, and connect with colleagues worldwide. The conference’s focus on being the best we can be, both as clinicians and as compassionate individuals, left a lasting impression. We eagerly await the next gathering in Berlin, ready to continue our journey of learning and growth.

Thursday Jun 16, 2016
Ep - 70 SMACC Dublin Day 2 Round Up.
Thursday Jun 16, 2016
Thursday Jun 16, 2016
Highlights from Day Two of SMACC: Exploring Leadership, Fear, and Compassion in Healthcare
Introduction
Welcome to the St. Emlyn's blog! We're Simon Carley and Natalie May, reporting from day two of the SMACC conference in Dublin. This day has been filled with engaging sessions, challenging ideas, and invaluable insights into various aspects of healthcare. From leadership and patient management to emotional resilience and compassion, the sessions have offered a deep dive into the complexities and challenges faced by healthcare professionals.
Ristola Ristup on Leadership and Gender Norms
The day started with Ristola Ristup's powerful plenary session on leadership. Ristup emphasized that leadership is a universal skill that transcends gender. She discussed the importance of both leadership and followership, stressing that everyone in healthcare needs to develop these skills. Her talk also highlighted the significance of mindful communication, noting that even brief comments can have a profound impact on others.
Ristup's insights into gender norms were particularly compelling. She argued that leadership should not be seen as a trait tied to gender but rather as a capability that everyone can and should cultivate. The discussion also covered the importance of creating a supportive environment where mentoring and sponsoring are integral parts of professional development.
Ross Fischer: Facing Fear in Medicine
Ross Fischer followed with a gripping talk on the fears that medical professionals face. He addressed the common anxieties that arise in healthcare, such as the fear of making mistakes and the emotional burden of patient outcomes. Fischer's storytelling was powerful, evoking a strong emotional response from the audience. He encouraged healthcare workers to confront their fears and use them as a source of strength and resilience.
Fischer suggested that his talk be viewed in a quiet setting to allow for personal reflection. His message emphasized that acknowledging fear is not a weakness but a vital step toward personal and professional growth. This session was a reminder that vulnerability is a natural part of the healthcare experience and that facing it can lead to greater compassion and understanding.
Ruben's Dre: Cultural Differences in Managing Agitated Patients
Ruben's Dre's session on managing agitated patients highlighted significant cultural differences in medical practice, particularly between the US and the UK. He discussed the use of physical restraints, a common practice in the US but rare in the UK. Dre's presentation was both humorous and insightful, challenging attendees to reconsider their practices and remain open to different approaches.
This session underscored the importance of cultural competence in healthcare. Dre emphasized the need to critically evaluate our practices and consider evidence-based alternatives. The discussion provided a valuable perspective on how different healthcare systems approach patient management, highlighting the importance of being adaptable and open-minded.
Liz Crow: The Power of Love and Compassion in Healthcare
Liz Crow delivered one of the most moving talks of the day, focusing on the role of love and compassion in healthcare. Crow argued that these "soft" skills are essential for effective patient care. She shared personal experiences from her work in pediatric ICU, emphasizing that empathy and compassion significantly impact patient outcomes.
Crow challenged the audience to consider how often they bring love and empathy into their professional roles. She noted that while healthcare providers may not frequently discuss these emotions, they are fundamental to the patient experience. Her talk highlighted an often-overlooked aspect of healthcare: the emotional and empathetic connection between providers and patients.
Concurrent Sessions: Diverse Topics and Key Insights
The afternoon offered a variety of sessions covering critical care, anesthetics, burnout, and more. Key topics included the risks associated with procedures in confined spaces, with a strong recommendation to avoid them whenever possible. This practical advice emphasized the importance of safety and preparedness in emergency situations.
Sueman Bizwaz's presentation blended humor with educational insights, reminding attendees of the value of engaging, entertaining education. Christina Henren's talk on the Boston attack response provided a sobering look at crisis management, while Mike Ebeneffi discussed the unique challenges of farm-related trauma in rural healthcare settings.
Bare-Knuckle Debates: A Showcase of Expertise
The bare-knuckle debates brought together experts to discuss controversial topics in emergency medicine. Simon Carley and Ryan Radecki highlighted recent research, while Carley and Scott Wein debated the "Fail Paradigm" in medicine. The debates were thought-provoking, exploring different perspectives on what constitutes failure and how it should be addressed.
Maxwell Wein and Chris Fox discussed the growing role of ultrasound in medical practice, debating its benefits and limitations. The final debate on thrombolyzing submassive PE featured compelling arguments from both sides, illustrating the complexities of clinical decision-making.
SMACC Ultrasonic: Fun and Learning Combined
The day concluded with the SMACC Ultrasonic, a fun and educational competition involving teams from Europe, Australia, and the USA. This event showcased the use of ultrasound in various clinical scenarios, providing a mix of competition and practical learning. The highlight was a playful demonstration involving an ultrasound and a leprechaun, emphasizing the innovative ways ultrasound can be taught.
Looking Ahead: SMACC 2024 in Berlin
The day ended with the exciting announcement that SMACC 2024 will be held in Berlin. The conference will take place in a unique venue with a round setup, promising a fresh and engaging experience. This setting is expected to inspire creativity and innovative presentations, continuing SMACC’s tradition of pushing the boundaries of medical education.
A Day of Insight and Reflection
Day two of SMACC was a rich exploration of the many facets of healthcare, from leadership and fear to the practicalities of patient management and the role of compassion. The sessions provided valuable insights and challenged attendees to think critically about their practices. As we look forward to the rest of the conference and the event in Berlin, we are reminded of the importance of continuous learning and empathy in our professional lives.
We hope you found this recap insightful and inspiring. Stay tuned for more updates, and as always, keep pushing the boundaries of what's possible in healthcare. Until next time, keep learning, keep caring, and stay inspired.

Tuesday Jun 14, 2016
Ep 69 - SMACC Dublin Day 1 Round Up
Tuesday Jun 14, 2016
Tuesday Jun 14, 2016
Day One Highlights from the Smack Dub Conference: A St Emlyns Overview
Welcome to the St Emlyns blog! We, Iain Beardsell and Simon Carley, are thrilled to report from the first day of the Smack Dub Conference in Dublin. It's been a while since our last update, and we're eager to share the day's experiences, which were filled with emotional moments, innovative presentations, and deep discussions. Here's a summary of the key events and takeaways.
Opening with a Tribute to John Hinds
The conference started early at 8 AM, with the opening session dedicated to the memory of John Hinds, a beloved figure in the Smack community who tragically passed away last year. Known for his engaging presentations and contributions to motorcycle medicine, John was greatly missed. The session began with Vic Brasel discussing the importance of feedback in medical education, setting the tone for a reflective and insightful day.
Meditation and Mindfulness in Medicine
Scott Weingart surprised the audience with a live podcast recording on meditation, an unusual topic for a resuscitation-focused conference. He emphasized the importance of mental exercise alongside physical health, advocating for practices like mindfulness to enhance well-being. Scott's discussion on Stoic philosophy and mental resilience resonated with many attendees, encouraging a broader perspective on personal and professional health.
Advances in Helicopter Emergency Medical Services
Gareth Davies from London Hems delivered a compelling talk on the evolution and future of helicopter emergency medical services (HEMS). He highlighted the ongoing campaign for an air ambulance in Northern Ireland, a cause John Hinds passionately supported. Gareth's discussion emphasized the need for moral authority to drive forward innovative healthcare solutions, especially in areas where traditional evidence can be challenging to gather.
Special Session: Remembering John Hinds
A particularly poignant session featured Janet, John's partner, who shared touching personal stories about John's life and work. Fred McSorley added humor with anecdotes from their time together in motorcycle medicine. This session provided a heartfelt tribute, capturing the essence of John's character and contributions. It concluded with a musical tribute, leaving many in the audience moved and inspired.
Diving Into the Main Conference
The day's formal sessions covered a range of topics, beginning with my talk on the future of emergency medicine. I discussed key factors such as political, demographic, and technological changes shaping the field. Demonstrating new technologies, we explored how these advancements could transform emergency medical practices.
Michelle Johnson's Vision of a Dystopian Medical Future
Michelle Johnson captivated the audience with her presentation on the dystopian future of emergency medicine. Drawing from literature, she explored potential ethical and societal implications of technological advancements in healthcare. Her talk challenged attendees to think critically about the future, offering a blend of caution and inspiration.
Addressing the Challenges of an Aging Population
Suzanne Mason focused on the increasing importance of geriatric care in emergency medicine. She discussed strategies for better managing the healthcare needs of an aging population, emphasizing comprehensive assessments and tailored interventions. Suzanne's talk highlighted the need for improved care models to address this growing demographic's unique challenges.
Diagnostic Processes: The Art of Thin Slicing
Swami's session on thin slicing in diagnosis delved into the cognitive processes behind decision-making in emergency situations. He explored how clinicians can refine their intuition and pattern recognition to improve diagnostic accuracy. This presentation underscored the importance of cognitive skills in high-pressure medical environments.
Afternoon Sessions: A Range of Engaging Topics
The afternoon featured a variety of sessions, with topics ranging from ECMO and Perimortem C-sections to discussions on the future of medical journals. One notable debate featured Jeff Drazen and Richard Smith discussing the evolving role of journals in the digital age. Richard Smith argued for a shift away from traditional publishing, advocating for more open-access models to democratize knowledge.
Live Demonstrations and Innovative Presentation Styles
The "Kickstart the Heart" session showcased a live demonstration of ECMO CPR, highlighting the innovative presentation styles encouraged at Smack. The diversity of approaches, from traditional lectures to interactive demonstrations, provided a rich learning experience.
Sarah Gray's talk on Perimortem C-sections emphasized the importance of preparedness for rare but critical interventions. The session highlighted the necessity of regular practice to ensure readiness in life-threatening situations.
Diverse Presentation Approaches
John Carlisle's creative presentation on detecting fraud in clinical trials used the perspective of his six-year-old daughter, making complex topics accessible and engaging. Meanwhile, Richard Smith's slide-free talk demonstrated the power of effective storytelling in conveying complex ideas, particularly his radical views on the future of medical journals.
Wrapping Up and Looking Ahead
The final session, which Simon participated in, focused on the future of knowledge dissemination. The discussion explored potential post-paper publication models and the increasing role of digital and social media in spreading medical knowledge. The panel highlighted the need for adaptability in a rapidly changing information landscape, with Richard Smith advocating for closing traditional journals in favor of open-access platforms.
As the day concluded, attendees reflected on the depth and breadth of content covered. While some enjoyed Dublin's nightlife, Simon and I prepared for our talks the following day, opting for a quiet evening.
Conclusion
Day one of the Smack Dub Conference was a remarkable success, filled with memorable tributes, innovative presentations, and deep discussions. The event challenged us to think critically about the future of emergency medicine and the role of various communication styles in medical education. We look forward to the rest of the conference and sharing more insights and experiences. Stay tuned to the St Emlyns blog for further updates and detailed session reviews. See you tomorrow!

Friday Apr 29, 2016
Ep 68 - An Englishman in South Africa with Robert Lloyd
Friday Apr 29, 2016
Friday Apr 29, 2016
Navigating Major Trauma in South Africa: An Unforgettable Experience
Introduction
Simon Cowie and Robert Lloyd bring a special episode from Cape Town, South Africa, at the International Conference of Emergency Medicine (ICEM). The focus is on Robert's profound experiences working in South Africa’s emergency departments, particularly dealing with major trauma in challenging environments like Khayelitsha Hospital. This blog post recounts Robert's transformative journey, offering insights into managing severe trauma cases and coping with intense psychological stress.
Experiencing Major Trauma in South Africa
Robert’s elective stint in South Africa aimed to deepen his expertise in major trauma, a specialty for which the country is well-known due to its high rates of violence-related injuries. He worked in New Somerset Hospital in the city and Khayelitsha Hospital in the township, where he faced a staggering volume of trauma cases, especially during "payday weekends"—a time marked by increased violence and accidents due to heightened alcohol consumption.
On his first night shift, Robert encountered an overwhelming number of severe cases, including 32 stab wounds to the chest, seven to the neck, and eight fatalities, six of whom were minors. This immediate immersion into high-stakes trauma care was a stark contrast to his previous experience in Australia and underscored the unique challenges faced by healthcare professionals in South Africa.
The Reality of Community Assaults
A particularly harrowing aspect of Robert’s experience was dealing with the aftermath of community assaults, where residents, in the absence of adequate police presence, took justice into their own hands. This vigilante justice often resulted in severe injuries, adding to the already heavy burden on emergency departments. Patients frequently presented with blunt trauma and crush injuries, showcasing the harsh realities of community-based violence and the critical need for comprehensive emergency care services.
Psychological Impact and Stress Management
The sheer volume and severity of cases led Robert to experience an acute stress reaction, referred to as "Condition Black," a term popularized by Dave Grossman in "On Combat." This state represents a high level of stress-induced impairment, where cognitive and physical functions degrade. Robert felt overwhelmed, his heart racing, hearing muffled, and hands shaking—making even simple medical procedures challenging. This response highlighted the necessity of managing psychological stress to maintain effective performance in high-pressure situations.
Strategies for Overcoming Psychological Barriers
To cope with the intense stress and improve his performance, Robert employed several strategies: overlearning essential skills, engaging in mental rehearsal, and fostering relentless positivity.
-
Overlearning Essential Skills: This involved practicing critical procedures like fast scanning and intercostal drain insertion until they became automatic. He also mastered surgical hand tying, crucial in the resource-limited setting of Khayelitsha Hospital, where suture instruments were often unavailable. This preparation ensured he could perform these tasks effectively, even under stress.
-
Mental Rehearsal: Robert used this technique to visualize and mentally practice the steps of critical procedures, such as rapid sequence intubation (RSI) for severe head injuries. This repeated mental walkthrough helped reduce anxiety and built confidence, making the actual procedures feel familiar and more manageable.
-
Relentless Positivity: Drawing from his experience as a competitive tennis player, Robert cultivated a positive mindset by replacing negative thoughts with positive affirmations. This approach helped him maintain focus and confidence, essential for handling the unpredictable and high-pressure nature of emergency medicine.
The Importance of Stress Inoculation Training
Robert’s experience underscored the value of stress inoculation training (SIT) in medical education. SIT involves gradually exposing individuals to stress in a controlled environment, helping them build resilience and improve their ability to handle high-pressure situations. This training is particularly beneficial for medical professionals, preparing them to remain calm and make sound decisions under stress. Incorporating SIT into medical simulations provides a safe yet realistic training ground for emergency scenarios, enhancing preparedness and performance.
Conclusion
Robert’s journey through South Africa’s emergency medicine landscape was a profound learning experience, highlighting the importance of comprehensive preparation in handling severe trauma cases. His strategies for managing psychological stress—overlearning, mental rehearsal, and maintaining positivity—proved invaluable. These methods not only improved his technical skills but also built the mental resilience needed to thrive in high-pressure environments.
The experience also highlighted the critical need for training programs like SIT to better prepare medical professionals for the realities of emergency medicine. Whether working in high-trauma settings like South Africa or less extreme environments, the lessons learned from managing stress and psychological preparedness are universally applicable.
Call to Action
For further insights into emergency medicine, visit Robert’s blog, Pondering EM, and follow him on Twitter @ponderingem. For those interested in exploring stress management in high-pressure situations, "On Combat" by Dave Grossman is a highly recommended read. Thank you for joining us on the St. Emlyns Podcast. Please subscribe and leave us a review to help us continue bringing valuable content to the medical community.

Wednesday Mar 23, 2016
Ep 67 - Intro to EM: Sepsis
Wednesday Mar 23, 2016
Wednesday Mar 23, 2016
## Navigating Sepsis in Emergency Medicine: Key Approaches and Insights
Sepsis is a life-threatening condition that occurs when the body's response to an infection injures its own tissues and organs. It is a complex and evolving challenge in emergency medicine, requiring prompt recognition and effective management. This blog post explores the fundamental steps for managing sepsis in the emergency department (ED), emphasizing early identification, appropriate treatment, and the importance of clinical judgment.
### The Complexity of Sepsis Management
Sepsis presents a unique challenge due to its variable presentation and potential severity. Patients may appear relatively stable upon arrival but can rapidly deteriorate if not managed promptly. Recent advancements have introduced new strategies and guidelines, such as the "sepsis six" and SOFA criteria, which are integral to medical education and practice in the UK. Despite these tools, sepsis management remains complex, necessitating a clear and straightforward approach in the ED.
### Early Recognition and Assessment
The initial assessment of a patient suspected of sepsis is critical. Time-sensitive interventions can significantly impact outcomes. For example, consider a typical scenario: a 50-year-old man with a recent cough, a temperature of 39°C, and a pulse rate of 120 arrives in the ED. Initial steps include taking the report seriously, preparing the team and necessary equipment, and promptly assessing the patient upon arrival.
Recognizing sepsis early involves identifying key signs such as fever, tachycardia, hypotension, and altered mental status. Standard criteria like SIRS (Systemic Inflammatory Response Syndrome) and QSOFA (Quick Sequential Organ Failure Assessment) help in early identification. SIRS focuses on physiological responses like temperature, heart rate, and white blood cell count, while QSOFA emphasizes mental status, respiratory rate, and blood pressure.
### Efficient Management through Concurrent Activity
In the ED, efficiency is paramount. Implementing a "concurrent activity" approach, where multiple interventions occur simultaneously, is essential. Upon receiving the patient, administer oxygen, attach monitoring equipment, and begin obtaining observations. The paramedic handover provides critical insights, including the patient's condition at the scene and any initial treatments administered.
Gathering a comprehensive history and conducting a physical examination are also crucial. This includes understanding recent symptoms, potential sources of infection, and any relevant medical history. Identifying the infection source helps tailor the treatment plan, ensuring that interventions are both appropriate and timely.
### The Role of Early Antibiotics
The timing and selection of antibiotics are pivotal in sepsis management. While there is a strong push for early administration of broad-spectrum antibiotics, it is equally important to choose the right antibiotic based on the suspected infection source. This requires a thorough patient assessment and adherence to local microbiology guidelines.
Antibiotic stewardship is vital to combat growing antibiotic resistance. Avoiding indiscriminate use of broad-spectrum antibiotics helps minimize the risk of resistance and side effects. For instance, a suspected urinary tract infection (UTI) requires different antibiotics compared to pneumonia. Clinicians must make informed decisions to provide effective treatment while preserving antibiotic efficacy.
### Objective Measures: SIRS, QSOFA, and Lactate
Objective measures complement clinical judgment in diagnosing and managing sepsis. The SIRS criteria, although useful, are not specific to sepsis and can be elevated in other conditions. QSOFA criteria, focusing on altered mental status, respiratory rate, and blood pressure, provide a more specific indication of sepsis severity and help identify high-risk patients.
Lactate levels are a valuable marker of tissue hypoperfusion and sepsis severity. Elevated lactate levels, particularly above 2 mmol/L, signal a need for aggressive intervention. However, lactate must be interpreted in the context of the entire clinical picture, as levels can be influenced by factors such as physical exertion or alcohol use.
### Treatment and Monitoring
Effective sepsis management involves prompt treatment and continuous monitoring. Key interventions include administering oxygen, ensuring adequate fluid resuscitation, and providing appropriate antibiotics. Fluid resuscitation, particularly with intravenous crystalloids, aims to restore tissue perfusion and prevent organ dysfunction.
Patients with persistent hypotension or altered mental status after initial resuscitation may require admission to a high-dependency unit (HDU) or intensive care unit (ICU). Early involvement of inpatient teams and clear communication across departments are crucial for comprehensive patient management. The goal is to stabilize the patient, address the underlying infection, and prevent complications.
### Avoiding Diagnostic Pitfalls
Not all patients with sepsis-like symptoms have sepsis. Conditions such as pulmonary embolism, myocardial infarction, and viral infections can mimic sepsis, necessitating careful differential diagnosis. Continuous reassessment, thorough investigations, and seeking second opinions are vital to avoid diagnostic errors and ensure appropriate treatment.
For example, a patient with fever, elevated heart rate, and respiratory distress may not have sepsis but rather a pulmonary embolism or acute coronary syndrome. Comprehensive evaluation, including appropriate diagnostic tests, helps clarify the diagnosis and guide treatment.
### The Importance of Clinical Judgment
While objective measures are essential, clinical judgment remains a cornerstone of sepsis management. Understanding the patient's symptoms, history, and overall presentation is critical. Asking the right questions, consulting with colleagues, and involving specialists when necessary enhances decision-making and patient care.
Involving family members in discussions can also provide valuable insights into the patient's baseline health and recent changes. Additionally, leveraging the expertise of specialists, such as infectious disease or critical care consultants, can help manage complex cases.
### The Evolving Landscape of Sepsis Management
Sepsis management is continually evolving, with new research and guidelines refining our approach. Staying informed through continuous education and engagement with current literature is crucial. Notable resources include EMCrit and Foamcast podcasts, which provide valuable updates on critical care topics, including sepsis.
Emerging areas of interest include biomarkers for diagnosis and prognosis, novel therapies, and advanced monitoring techniques. Understanding these developments helps clinicians stay at the forefront of sepsis care and improve patient outcomes.
### Conclusion: Making a Difference in Sepsis Care
Sepsis is a formidable challenge in emergency medicine, but with prompt recognition and appropriate treatment, patient outcomes can be significantly improved. Emergency physicians play a critical role in identifying sepsis early, initiating lifesaving treatments, and collaborating with colleagues for comprehensive care. By maintaining a high index of suspicion, utilizing objective criteria alongside clinical judgment, and staying abreast of the latest developments, healthcare providers can make a real difference in the lives of their patients.
As you approach your next shift, remember these principles. Identify at-risk patients, initiate timely interventions, and follow up on their outcomes. This ongoing process of learning and application not only sharpens clinical skills but also enhances patient care. We hope this blog post has provided valuable insights and practical guidance. Please share your experiences and thoughts in the comments below, and stay tuned for more updates from the St. Emlyns team. Together, we can continue to improve our practice and provide the best possible care for our patients.

Wednesday Feb 24, 2016
Ep 66 - When Professional and Personal Worlds Collide with Liz Crowe
Wednesday Feb 24, 2016
Wednesday Feb 24, 2016
Navigating Personal and Professional Boundaries in Healthcare
In this St. Emlyns blog post, Iain Beardsell and Liz Crowe discuss the challenging scenarios healthcare professionals face when their personal and professional lives intersect, particularly in emergency and critical care settings. These situations are complex, requiring careful navigation to maintain ethical standards and patient confidentiality.
Understanding Dual Roles
Healthcare professionals often encounter situations where they have a personal connection with a patient. This could be someone they know vaguely, a close friend, or even a family member. Such instances require careful reflection on whether to act as a friend or a professional. It's crucial to declare any personal connections to colleagues and maintain a clear boundary to ensure unbiased care. The primary duty in these cases is to the patient's confidentiality, regardless of personal ties.
Case Study: Community Members as Patients
A hypothetical scenario is presented where a child from the same school attended by a healthcare professional's children is admitted following a trauma. This situation exemplifies the conflict between professional responsibilities and community ties. Even if the professional knows the community, sharing patient details without consent is unethical. It's important to resist the urge to share information, even when under pressure from friends or community members. The first response should always prioritize the patient's confidentiality and respect for their family's wishes.
Handling Situations Involving Close Friends or Family
When the patient is a close friend or family member, the complexity intensifies. The key is to establish clear boundaries and communicate openly with the healthcare team. If possible, the professional should hand over care to another team member to avoid conflicts of interest. This separation helps prevent emotional turmoil and ensures the patient receives unbiased care. In emergencies where immediate care is needed, the professional should still step back as soon as feasible.
Managing the Desire for Information
Healthcare professionals may feel a natural curiosity about the condition of someone they know personally. However, accessing medical records or sharing information without a professional need is a breach of confidentiality. Professionals must remind themselves that they have no right to this information if not directly involved in the patient's care. The ethical responsibility includes abstaining from looking at records or discussing the patient's condition unless explicitly authorized.
When a Colleague Becomes a Patient
The situation becomes particularly sensitive when the patient is a colleague. This could involve anything from minor injuries to serious, life-threatening conditions. The emotional dynamics in the team can complicate care delivery. It is essential to maintain professionalism, avoid gossip, and ensure that any shared information is with the patient's consent. After the initial crisis, it is vital for the team to discuss how to handle the situation moving forward, including managing information dissemination within the department.
Tragic Outcomes: Death of a Colleague
A particularly difficult scenario is when a colleague passes away while under the care of the healthcare team. This rare event requires a compassionate and professional response. The focus should initially be on supporting the family and the team. Management should be informed immediately, and additional support staff may be needed to maintain department function. A formal debriefing process should be arranged to help the team process the event and plan memorials or support for the family.
The Role of Social Media
In the digital age, social media presents additional challenges for maintaining patient confidentiality. Even vague posts about work events can be considered breaches of confidentiality and may result in disciplinary action. Healthcare professionals must be cautious about accepting friend requests or communicating with patients or their families on social media. Maintaining professional boundaries is essential, and any communication should respect privacy laws and ethical standards.
Conclusion: Upholding Professionalism and Confidentiality
Navigating the intersection of personal and professional lives in healthcare requires strict adherence to ethical standards. Whether dealing with community members, friends, family, or colleagues, the primary responsibility is to maintain patient confidentiality and uphold professional integrity. These situations are challenging, but clear boundaries and proactive planning can protect both the patient and the professional.
Healthcare professionals are encouraged to reflect on these issues and discuss them with their teams. Seeking guidance from senior colleagues and maintaining open communication are key strategies in managing these situations. Patient confidentiality must always be a priority, and maintaining professional boundaries is crucial for sustaining trust and integrity in healthcare.
Key Takeaways:
- Always prioritize patient confidentiality and ethical standards.
- Declare personal connections to patients and avoid involvement in their care.
- Refrain from accessing information or discussing patients without professional necessity.
- Use caution with social media to avoid breaches of confidentiality.
- Plan ahead for handling complex situations involving personal and professional overlap.
This post aims to provide insights into managing the delicate balance between personal and professional responsibilities in healthcare, emphasizing the importance of maintaining professionalism and confidentiality at all times.

Thursday Feb 04, 2016
Ep 65 - The management of Paediatric trauma in the UK with Ross Fisher
Thursday Feb 04, 2016
Thursday Feb 04, 2016
Ross Fisher, consultant paediatric surgeon and lead for TARNlet joins Simon Carley at the London Trauma Conference to discuss the challenges in managing paediatric trauma in the UK.
Monday Jan 25, 2016
Monday Jan 25, 2016
Sandra Viggers and Vic Brazil grace St.Emlyn's with a conference report from Sand Diego and the
International Meeting for
Simulation in Healthcare (IMSH) #IMSH2016.

Wednesday Jan 13, 2016
Ep 63 - The Role of UK Trauma Units with Tim Coates (LTC)
Wednesday Jan 13, 2016
Wednesday Jan 13, 2016
Iain Beardsell joins Tim Coats, chair of the UK Trauma Audit Network, to discuss the role of trauma units within major trauma networks.

Wednesday Dec 30, 2015
Ep 62 - The role of paediatric surgeons in trauma with Ross Fisher (LTC)
Wednesday Dec 30, 2015
Wednesday Dec 30, 2015
Simon and Ross Fisher from Sheffield discuss the emerging role of paediatric surgeons in trauma. This podcast was recorded at the London Trauma Conference (so sorry for a bit of background noise at times).
vb
S
Thursday Dec 17, 2015
Ep 61 - Grief at Christmas with Liz Crowe
Thursday Dec 17, 2015
Thursday Dec 17, 2015
In this episode of the St Emlyn's podcast, Iain Beardsall and Liz Crowe discuss the unique challenges healthcare professionals face during the Christmas season in emergency and intensive care settings. They delve into how to balance the festive atmosphere with the stark reality of dealing with tragic events, offering practical advice on effective communication and self-care. The conversation emphasizes the importance of acknowledging the season while maintaining professional decorum, the role of humour and camaraderie in the workplace, and strategies for transitioning from work back to family life.
This episode is particularly valuable for doctors, nurses, and medical students seeking to navigate the emotional complexities of working during the holiday season.
00:00 Introduction and Festive Season Challenges
01:05 Acknowledging the Festive Season in Healthcare
02:12 Communicating Bad News During Christmas
04:49 Balancing Work and Personal Life During Festive Times
09:20 Finding Joy and Humor Amidst Challenges
12:09 Conclusion

Wednesday Dec 09, 2015
Ep 61 - Londoon Trauma Conference 2015 Day 2 Summary
Wednesday Dec 09, 2015
Wednesday Dec 09, 2015
Our summary of Day 2 of the excellent London Trauma Conference. A unique threesome from Nat, Simon and Iain.....

Tuesday Dec 08, 2015
Ep 60 - Londoon Trauma Conference 2015 Day 1 Summary
Tuesday Dec 08, 2015
Tuesday Dec 08, 2015
Greetings from the London Trauma Conference!
As has become our pre-Christmas custom, Iain and I have been hanging out at the fabulous London Trauma Conference, hearing about advances and controversies in trauma care and tracking down some of the speakers to find out exactly what they really think (and recording it, for podcasts we'll release in due course).
The conference extends over four days, incorporating the Air Ambulance and Prehospital Day and the Cardiac Arrest Symposium; unfortunately we can't stick around for those but our colleagues over at the RCEM FOAM network will be podcasting from those days too, so keep an eye on their site and podcast feed too.
Friday Dec 04, 2015
Ep 59 - Lessons learned from the November Paris attacks with Youri Yordanov
Friday Dec 04, 2015
Friday Dec 04, 2015
We are truly honored to listen and learn from Dr Youri Yordanov from Paris. Youri was the senior emergency physician on duty on the 13/11/15 during the brutal and terrifying terrorist attacks in Paris. Here he joins St.Emlyn's to discuss how they managed a mass casualty incident with lessons for us all.
There is no doubt that without the skills, preparation and response of Youri, his ED team, the wider hospital and the emergency service in general the death rate would have been much worse.
Thanks Youri for your wisdom and reflections.
vb
S

Saturday Nov 28, 2015
Ep 58 - Clinical Judgement for the Emergency Physician
Saturday Nov 28, 2015
Saturday Nov 28, 2015
My talk from the RCEM conference in Manchester 2015.
Linked blog post here. http://stemlynsblog.org/making-good-decisions-in-the-ed-rcem15/
Slides are here http://www.slideshare.net/simoncarley7/making-good-decisions-rcem-2015-manchester-wednesday
Have fun and enjoy your emergency medicine.
S

Monday Nov 02, 2015
Ep 57 - When things go wrong - the difficult conversation
Monday Nov 02, 2015
Monday Nov 02, 2015
Simon and Nat talk about how to have that tricky conversation when you have to tell a colleague that they may have made a mistake.
vb
S

Sunday Sep 27, 2015
Ep 56 - Intro to EM: How to refer a patient
Sunday Sep 27, 2015
Sunday Sep 27, 2015
Mastering the Art of Clinical Referrals: A Guide for Emergency Physicians
Introduction
Effective communication is crucial in the emergency department (ED), particularly when referring patients to inpatient teams. It not only ensures optimal patient care but also enhances professional relationships and personal job satisfaction. In this post, inspired by the St. Emlyns podcast, we'll explore a practical framework for making clinical referrals, emphasizing the importance of clear, structured communication. We'll discuss the SBAR (Situation, Background, Assessment, Recommendation) format, the concept of the "James Bond opening," and strategies for handling difficult conversations, all tailored to the fast-paced environment of emergency medicine.
Why Effective Referrals Matter
Referrals are an integral part of patient management in the ED. Every referral is made with the patient's best interest in mind, whether they need further investigations, specialized treatment, or simply continuity of care. Ensuring that the receiving team understands the urgency and context of the referral is vital. Good communication can influence how the inpatient team perceives the referring physician and can enhance collaborative relationships, leading to better patient outcomes and professional fulfillment.
Setting the Stage: The James Bond Opening
When initiating a referral, it’s essential to grab the attention of the receiving team quickly and effectively. This is where the "James Bond opening" comes in—start with a high-impact statement that summarizes the critical aspect of the patient's condition. For example, instead of saying, "I have a patient with abdominal pain," begin with, "I have a 25-year-old male who likely has appendicitis." This approach not only captures attention but also sets the stage for a focused and efficient conversation.
The SBAR Framework: Structuring Your Referral
The SBAR model provides a structured approach to communication, ensuring all essential information is conveyed succinctly. Here’s how to implement it:
Situation
Begin with a brief description of the patient's current condition. This is where the "James Bond opening" fits perfectly. Clearly state the key clinical concern that necessitates the referral.
Background
Provide context for the situation. This includes relevant medical history, the reason for the current ED visit, and any pertinent findings. For instance, you might say, "The patient has had two days of right iliac fossa pain and a history suggestive of appendicitis."
Assessment
Share your clinical judgment about the patient's condition. This not only demonstrates your understanding but also signals the expected pathway of care. In our example, "Based on the examination and symptoms, I believe the patient has appendicitis."
Recommendation
Conclude with a clear, direct request. Specify what you need from the inpatient team, such as a physical assessment, further diagnostic testing, or specific interventions. For instance, "I'd appreciate it if the surgical team could evaluate the patient for potential appendicitis and consider admission for further management."
Enhancing the Referral Process: Tips and Tricks
Introduce Yourself Clearly
Always start the conversation by introducing yourself with your name and role. For example, "Hi, I'm Ian, one of the ED doctors." This personal touch helps build rapport and sets a friendly tone. If the receiving team introduces themselves by title only, politely ask for their name, fostering a more personable interaction.
Predict and Prepare for Questions
Anticipate the questions the receiving team might ask and prepare your responses. For example, if referring a potential appendicitis case, be ready to discuss symptoms, lab results, and physical findings. This not only streamlines the conversation but also demonstrates your preparedness and competence.
Use the Illusion of Choice
To smooth the referral process, offer options that guide the receiving team towards a decision that benefits the patient. For instance, "Would you prefer to see the patient in the ED or on the ward?" This technique, known as the illusion of choice, empowers the receiver while subtly directing the conversation towards the desired outcome.
Navigating Difficult Conversations
Not all referral conversations go smoothly. Sometimes, the receiving team may be uncooperative or dismissive. Here are strategies to handle such situations:
Stay Calm and Professional
If the conversation becomes contentious, avoid escalating the situation. Remain calm and professional, focusing on patient care rather than engaging in arguments. A useful tactic is to suggest pausing the conversation: "Let me discuss this further with my senior and get back to you."
Seek Support from Senior Staff
If you encounter resistance, consult a senior colleague or consultant. They can provide additional insights or take over the conversation, ensuring the patient receives the necessary care.
Empathize with the Receiving Team
Understand that the receiving team might be under significant pressure, dealing with their own caseloads and challenges. Acknowledging their situation can defuse tension and facilitate a more constructive dialogue.
Conclusion: Practice Makes Perfect
Effective referrals are a skill that, like any other medical procedure, requires practice and reflection. Using the SBAR framework, starting with a strong "James Bond opening," and preparing for potential questions can significantly improve the quality of your referrals. Remember, every interaction is an opportunity to enhance patient care and build professional relationships.
For more insights and discussions on emergency medicine, communication skills, and more, visit the St. Emlyns blog and podcast series. Let's continue to improve our skills and ensure the best outcomes for our patients.

Saturday Sep 05, 2015
Ep 55 - Communicating (not Breaking) Bad News with Liz Crowe
Saturday Sep 05, 2015
Saturday Sep 05, 2015
Communicating Difficult News in Emergency Medicine: A Guide from St Emlyns
Introduction
Effective communication of difficult news is a critical skill in emergency medicine. This guide, based on a discussion between Iain Beardsell and Liz Crowe, explores best practices for delivering challenging information to patients and their families, emphasizing compassion and clarity.
The Importance of Language
The terminology used when delivering bad news can significantly impact the recipient's perception. Liz Crowe suggests avoiding phrases like "delivering bad news" or "breaking bad news," as they imply a one-time transaction. Instead, "communicating difficult news" emphasizes an ongoing process that includes listening, support, and engagement. This language shift helps set a compassionate tone and encourages continuous dialogue, reassuring families that they are not alone.
Building a Supportive Relationship
The goal of communicating difficult news is not just to convey information but to build a supportive relationship. Unlike a delivery person who leaves after a transaction, healthcare professionals should remain engaged, ensuring that families feel heard and supported. This involves being present, offering a listening ear, and providing continuous support, which helps families process the news and feel significant during a difficult time.
Self-Awareness in Communication
Healthcare professionals must be self-aware of their emotions and biases when delivering difficult news. Liz points out that under stress, professionals might default to using medical jargon, which can distance them from the family. Recognizing one's emotional triggers and managing them is crucial for maintaining a compassionate demeanor. Self-awareness also involves understanding personal limitations and seeking support when needed, ensuring that caregivers can provide the best possible support to families.
Creating the Right Environment
The environment where the news is delivered plays a crucial role. A private, quiet space where everyone can sit comfortably helps create a sense of safety and respect. Healthcare professionals should take a moment to prepare mentally before the conversation, organizing their thoughts and emotions. This preparation helps in delivering the news clearly and calmly, reducing the chances of miscommunication.
Nonverbal Communication and Setting the Tone
Nonverbal cues, such as facial expressions and body language, significantly influence the tone of the conversation. Professionals should approach with a serious and empathetic demeanor, setting the expectation for a difficult conversation. A somber expression can help prepare families for the news, as opposed to a smile, which might create false hope. The first and last things said are particularly memorable, so they should be chosen carefully to ensure clarity and compassion.
Clarity and Honesty
Clarity is paramount when delivering difficult news. If a patient has died, it is essential to state this clearly and directly, avoiding euphemisms and medical jargon. Information should be given in small, digestible pieces, allowing families to process it. Professionals should also be prepared to repeat or clarify information, as initial shock can make it difficult for families to absorb all details.
Handling Emotional Reactions
Emotional reactions are natural and expected. Liz advises against immediately offering tissues, as this can imply discomfort with the family's grief. Instead, give them space to express their emotions. Healthcare professionals should be prepared for a range of responses, from tears to anger, and maintain a supportive presence throughout. Validating the family's emotions is crucial, as is allowing them time to grieve.
Continuous Engagement and Follow-Up
The conversation should not end after delivering the news. Continuous engagement is vital, including checking in with the family periodically and being available for follow-up questions. This ongoing support helps families feel cared for and reassures them that they are not left to navigate the situation alone. Follow-ups can include arranging further meetings, providing written materials, or referring to counseling services.
Special Considerations for Children
When children are involved, the information should be age-appropriate and delivered with care. Liz suggests involving children in the conversation, as excluding them can lead to confusion and mistrust. It is essential to use simple, clear language and to be honest about the situation. Reassuring children that it is okay to feel sad or confused helps them process their emotions.
Respecting Cultural and Religious Beliefs
Cultural and religious beliefs can significantly influence how families perceive and process difficult news. Healthcare professionals should respect these beliefs and tailor their communication accordingly. This might involve understanding specific rituals or customs and involving spiritual advisors when appropriate. Respecting these practices provides comfort and shows respect for the family's values.
Conclusion
Communicating difficult news is a challenging but essential aspect of emergency medicine. It requires empathy, clarity, and a commitment to ongoing support. By focusing on these elements, healthcare professionals can help families feel supported and understood during some of the most challenging moments of their lives. The insights shared by Liz Crowe and Iain Beardsell emphasize the importance of a compassionate and structured approach, ensuring that these conversations are handled with the utmost care and respect.
For more insights on navigating complex topics in healthcare, stay tuned to the St Emlyns blog. We are committed to providing valuable information to support healthcare professionals in their journey of delivering compassionate and effective care.

Sunday Jul 26, 2015
Ep 54 - Intro to EM: Analgesia in the ED.
Sunday Jul 26, 2015
Sunday Jul 26, 2015
Iain and Simon discuss the core skills that all EM clinicians need to manage pain in the ED.
These are the basics, but don't be put off. The basics are more important than the fancy stuff that we will discuss in a later podcast.
vb
S

Thursday Jul 16, 2015
Ep 54 - A tribute to John Hinds
Thursday Jul 16, 2015
Thursday Jul 16, 2015
A podcast mini to round up and look forward to the next few months on the podcast.
We also have a special recording of Danny Boy from the Irish Youth Choir and conducted by Greg Beardsell. This performance was dedicated to Dr John Hinds in Dublin following his untimely death in a motorcycle accident.
Please listen and take a moment to remember him and all that he has done to inspire everyone involved in the care of the injured.
vb
S
Sunday Jul 12, 2015
Ep 53 - Day 2 and 3 Round Up (SMACCUS)
Sunday Jul 12, 2015
Sunday Jul 12, 2015
Day 2 and 3 at #smaccUS. Iain and Simon round up the highlights and look forward to #smaccDUB.
S

Tuesday Jul 07, 2015
Ep 52 - Managing grief in the ED with Liz Crowe
Tuesday Jul 07, 2015
Tuesday Jul 07, 2015
Navigating Grief: Lessons from the St Emlyns Podcast with Liz Crow
In a compelling episode of the St Emlyns podcast, host Ian Bidsel engages in a profound discussion with pediatric social worker Liz Crow about the intricacies of grief, especially within the healthcare sector. This episode was prompted by the tragic loss of John Hines, a respected member of the SMACC community known for his work as a motorcycle doctor. Liz shares her insights into the unique challenges faced by healthcare professionals when dealing with grief, both personally and professionally.
The Unique Nature of Grief
Grief is a deeply personal experience that varies significantly from person to person. Liz Crow emphasizes that there is no "normal" way to grieve; each individual's response is shaped by various factors, including age, personality, and prior experiences with loss. The podcast challenges the traditional Kubler-Ross model, which suggests a linear progression through five stages of grief. Liz argues that grief is a fluid process without a set path, characterized by an unpredictable mix of emotions.
Grieving in the Healthcare Profession
Healthcare professionals often encounter death and suffering, which can complicate their grieving process. The sudden death of John Hines highlighted the vulnerabilities even within a community accustomed to dealing with trauma. Liz and Ian discuss the common practice of compartmentalization among healthcare workers, where emotions are set aside to focus on the task at hand. While this can be a necessary coping mechanism, Liz warns against prolonged avoidance of emotions, as it can lead to long-term psychological issues.
The conversation underscores the importance of self-awareness and self-care. Healthcare professionals are encouraged to acknowledge their grief and seek support when necessary. This may involve adjusting work responsibilities or taking time off to process emotions. Liz stresses that compartmentalization should be temporary and that healthcare workers need to find safe spaces to express and process their grief.
Coping Strategies and Community Support
Liz explores various coping strategies that can help individuals navigate their grief. These include journaling, physical activity, creative expression, and talking with trusted friends or professionals. The key is to find what works best for each person. The SMACC and FOAMed communities provide a supportive network, especially through social media, which has facilitated shared experiences and mutual support. However, Liz notes that online interactions can sometimes lack the depth needed for processing complex emotions.
The podcast also addresses the public aspect of grieving, particularly when the person lost is a public figure like John Hines. For those who admired him, his death serves as a stark reminder of life's fragility. Liz and Ian discuss the discomfort of confronting mortality, especially when it involves someone perceived as larger than life. This public grieving can add another layer of complexity to personal mourning.
The Importance of Open Conversations About Grief
A significant theme in the podcast is the need for open dialogue about grief. Liz encourages listeners to communicate their feelings and to be open about their vulnerabilities. She highlights the cultural stigma against showing emotion, particularly among men, and calls for a shift in how we perceive emotional expression. The healthcare community, often valuing emotional resilience, may need to rethink its attitudes toward vulnerability.
Ian shares his personal experiences of feeling isolated in his grief, particularly in professional settings where the expectation is to maintain a façade of normalcy. Liz acknowledges this common experience and emphasizes the importance of finding supportive communities and being open about one's struggles.
Integrating Grief into Life
Liz suggests that instead of viewing grief as something to "move through," it should be seen as an experience to integrate into one's life. She uses the metaphor of grief as a wound that eventually becomes a scar—while the initial pain may subside, the impact of the loss remains. This perspective encourages compassion for oneself and others, recognizing that grief is an ongoing process rather than a problem to be solved.
For those struggling to cope, Liz recommends seeking professional help, particularly if grief begins to manifest as clinical depression. She distinguishes between the natural process of grief and the symptoms of depression, advising individuals to seek support if they find themselves unable to manage their emotions.
The Role of Professional Support and Self-Care
The podcast highlights the critical role of professional support and self-care for healthcare workers. Liz discusses the importance of accessing supervision and counseling, especially during personal crises. Self-care is not a luxury but a necessity, particularly for those in caregiving roles who may prioritize others' needs over their own. This can include taking time off, engaging in hobbies, or simply allowing oneself to grieve.
Moving Forward with the Community
As the SMACC and FOAMed communities continue to process John Hines' loss, this podcast serves as a reminder of the collective nature of grief and the importance of community support. The conversation provides valuable insights into the complexities of grieving, the significance of open dialogue, and the power of mutual support.
In conclusion, Liz and Ian emphasize that grief is a natural part of life, much like happiness. They encourage listeners to approach their grief with gentleness and understanding, acknowledging that there is no right or wrong way to grieve. Whether through professional support, personal coping strategies, or community connections, the journey through grief is unique to each individual. The key takeaway is to be patient with oneself and others, recognizing that healing is a gradual and ongoing process.
This episode of the St Emlyns podcast offers a deep exploration of grief, providing practical advice and emotional support for those navigating this challenging experience. The conversation encourages healthcare professionals and the wider community to engage openly with their emotions and to support one another through the journey of grief.

Thursday Jun 25, 2015
Ep 51 - Day One Round Up (SMACCUS)
Thursday Jun 25, 2015
Thursday Jun 25, 2015
The first day of #smacc15 was amazing. An incredible introduction and an amazing program.

Wednesday Jun 24, 2015
Ep 50 - All in a day's work (SMACC 2015)
Wednesday Jun 24, 2015
Wednesday Jun 24, 2015
In this episode of the St Emlyn's podcast, Simon Carley and Iain Beardsell share insights from the SMACC 2015 conference in Chicago, focusing on the holistic experience of being a clinician. Ian delves into a personal and poignant case involving a 14-year-old boy named Charlie, who tragically died from traumatic injuries. Ian discusses the profound emotional impact this case had on him, the lingering doubts it created, and how it influenced his professional and personal life. This episode highlights the emotional challenges faced by emergency medicine practitioners and underscores the importance of mental resilience, compassionate communication, and self-care.

Wednesday Jun 24, 2015
Ep 49 - SMACC Workshops Review and Pearls
Wednesday Jun 24, 2015
Wednesday Jun 24, 2015
SMACC Chicago: Insights, Learning, and Community at St Emlyn's
The SMACC (Social Media and Critical Care) Conference in Chicago brought together healthcare professionals and thought leaders from around the world. The St Emlyn's team, comprising Iain Beardsell, Simon Carley, Rick Boddy, and Natalie May, participated in various workshops and sessions, sharing their experiences and insights. This blog post captures the essence of the conference, highlighting key learning outcomes and the vibrant community spirit.
Evidence-Based Medicine: From Theory to Practice
Simon Carley kicked off the day with a workshop titled "Gambling with the Evidence," focusing on practical applications of evidence-based medicine (EBM). Unlike traditional EBM sessions that often dwell on statistics and literature reviews, this workshop emphasized how to translate evidence into clinical practice. Simon, alongside Rick Boddy, Rob McSweeney, Ken Milne, and Rory Spiegel, explored how healthcare professionals manage the overwhelming volume of evidence and integrate it into their practice.
Key takeaways included strategies for storing and accessing evidence efficiently, influencing colleagues with evidence-based practices, and the importance of critical skepticism. The workshop stressed the responsibility of individuals to thoroughly understand the evidence before implementing changes in clinical settings. This session underscored the necessity of a balanced approach to adopting new practices, ensuring they are rooted in a comprehensive understanding of available evidence.
FOAM: Creating and Sharing Educational Content
Natalie May joined other prominent figures in the FOAM (Free Open Access Meducation) community for the "Brew Your Own FOAM" session. Alongside Salim Rezé, Rob Rogers, Haney Malamarts, and others, Natalie discussed the creation of blogs, podcasts, and other educational resources. The session, likened to an Apple bar, provided an informal yet informative platform for attendees to engage with experienced content creators.
Participants gained insights into the technical and creative aspects of producing FOAM content. The session encouraged the sharing of knowledge and resources, emphasizing that a diverse range of voices and perspectives enriches the medical community. Natalie highlighted the importance of FOAM in democratizing medical education, making high-quality information accessible to a global audience.
Exploring Chest Pain and Cardiology Pathways
Rick Boddy delved into the nuances of chest pain management and cardiology in his workshops. The morning session on evidence-based medicine included discussions on the values and outcomes in clinical trials, particularly concerning stroke and thrombolysis. Rick emphasized the varying perspectives of patients, doctors, and policymakers, stressing the importance of considering these viewpoints when evaluating clinical outcomes.
The afternoon's emergency cardiology workshop, featuring experts like Steve Smith and Louise Cullen, focused on chest pain pathways. The session covered a range of topics, from ECG interpretation to chest pain algorithms. Rick noted the growing interest in high-sensitivity troponins and the need for tailored chest pain pathways that cater to specific local populations. The discussion also addressed the challenges of implementing standardized pathways and the importance of trusting the evidence.
Getting Creative: Enhancing Communication Skills
Simon Carley also participated in a workshop titled "Getting Creative," which explored creative communication methods in the medical field. The workshop featured three sessions: Michelle Johnson on writing, Grace Slyo on visual presentations, and Rob Rogers on podcasting. Michelle Johnson, a skilled writer, guided participants through the art of crafting compelling narratives, particularly for blog posts. She emphasized the power of language and the importance of clear, concise communication.
Grace Slyo's session focused on improving visual communication, offering tips on graphic design and effective presentation techniques. She provided valuable resources and exercises to help participants enhance their visual storytelling skills. Rob Rogers concluded the workshop with practical advice on creating engaging podcasts, covering everything from content creation to technical aspects. Simon found the workshop incredibly valuable, noting that these skills are essential for effective knowledge dissemination in the medical community.
Pediatric Critical Care: Lessons and Strategies
Natalie May attended the SMACC mini session on pediatric critical care, where experts discussed managing critically ill children in emergency and intensive care settings. The session opened with Fran Lockey and Phil Hyde addressing pediatric airway and breathing management. They emphasized the importance of simple airway maneuvers and two-handed bag-valve-mask ventilation, debunking the myth that intubation is always necessary.
Lisa McQueen provided a poignant presentation on children in shock, referencing the case of Rory Staunton, a child who tragically died from sepsis after being discharged from the emergency department. The session highlighted the critical role of thorough reassessment and face-to-face evaluations in pediatric care. The importance of vigilance in monitoring children's progress before discharge was a key message.
Pre-Hospital Care: Excellence in Action
Iain Beardsell shared his experience from the pre-hospital care workshop, led by Carol Harbig from Greater Sydney Hems. The workshop featured a range of topics and speakers, providing an in-depth look at pre-hospital emergency medicine. The highlight of the day was a presentation by Ashley Leibig, who delivered a powerful talk on the emotional challenges faced by pre-hospital care providers and the importance of peer support.
Iain emphasized the value of visualization and mental rehearsal in preparing for high-stress situations. The workshop underscored the importance of practicing difficult scenarios mentally to ensure readiness when faced with real-life emergencies. This approach helps clinicians develop a clear action plan, reducing the likelihood of hesitation or error during critical moments.
The SMACC Community: Beyond Clinical Knowledge
One of the standout features of the SMACC Conference is its holistic approach to medical education. The conference not only covers clinical and technical topics but also addresses the emotional and psychological aspects of healthcare. Ashley Leibig's talk, reminiscent of Liz Crowe's impactful presentations, reminded attendees of the need for compassion and self-care in a field often dominated by high-stakes decision-making.
The conference provided ample opportunities for networking and community building. The St Emlyn's team noted the importance of connecting with peers, sharing experiences, and learning from each other. The collaborative spirit of the FOAM community was palpable, with participants eager to exchange ideas and support one another in their educational endeavors.
Preparing for the Big Stage: Final Thoughts
As the day drew to a close, the St Emlyn's team prepared for their presentations at the conference. The anticipation and nerves were palpable, reflecting the high regard in which the opportunity to speak at SMACC is held. The team emphasized the importance of thorough preparation, including practicing presentations and ensuring all details are in order.
The St Emlyn's team encouraged attendees and followers to engage with them, highlighting the value of these interactions in enriching the conference experience. They looked forward to meeting new people and deepening connections within the medical community.
Conclusion
The SMACC Conference in Chicago provided a rich and varied learning experience for the St Emlyn's team. From evidence-based medicine to pediatric critical care and pre-hospital medicine, the workshops offered valuable insights and practical knowledge. The conference also underscored the importance of creative communication, emotional resilience, and community support in the medical field.
For those unable to attend, the St Emlyn's team hopes this blog post offers a glimpse into the vibrant and dynamic environment of SMACC. The team is committed to sharing the knowledge and experiences gained at the conference, contributing to the broader medical community's growth and development.
As always, the St Emlyn's team encourages feedback and engagement from their readers. Whether you're interested in evidence-based medicine, FOAM, pediatric care, or any other topic, there's something for everyone in the rich tapestry of SMACC. Stay tuned for more updates and insights as the conference continues to unfold.

Thursday Jun 04, 2015
Ep 48 - Intro to EM: The patient with back pain.
Thursday Jun 04, 2015
Thursday Jun 04, 2015
Managing Back Pain in the Emergency Department: A Comprehensive Overview
In the emergency department (ED), back pain, particularly lower back pain without a traumatic cause, is a common and complex presentation. This condition can range from benign to life-threatening, requiring a thorough and systematic approach to ensure accurate diagnosis and effective management.
The Challenge of Back Pain in Emergency Medicine
Back pain patients often come with preconceived notions, especially when they seek pain relief. However, it's crucial to avoid jumping to conclusions, as back pain can result from various underlying issues, including serious conditions like ruptured abdominal aortic aneurysms (AAA) or infections. Therefore, clinicians should avoid hastily labeling cases as "musculoskeletal" without thorough evaluation.
Key Diagnostic Considerations
1. Broad Differential Diagnosis:
The differential diagnosis should begin with more severe and potentially life-threatening conditions. For example, an AAA can present with subtle back pain, particularly in the elderly, and missing this diagnosis can be catastrophic. Hence, abdominal examinations and bedside ultrasounds are essential tools for detection.
2. Pain Chronology and Characteristics:
Understanding the pain's duration and nature is vital. Chronic pain may suggest long-standing issues, while acute pain can indicate new, potentially severe conditions. Atypical symptoms like pain that worsens at night or at rest, as opposed to musculoskeletal pain that improves with rest, could signal neoplastic or infectious processes.
3. Multi-System Evaluation:
A comprehensive assessment, including vital signs and a review of systems, is critical. For instance, signs like tachycardia, fever, or hypotension can indicate systemic issues such as sepsis. Conditions like pyelonephritis, especially in immunocompromised patients, can manifest as back pain, necessitating a thorough evaluation.
Specific Conditions and Red Flags
Ruptured Abdominal Aortic Aneurysm (AAA):
In elderly patients, AAA must always be considered, especially with sudden onset back pain. This condition can be rapidly fatal, and quick diagnosis via ultrasound is crucial.
Neoplastic Disease:
Symptoms such as unexplained weight loss, persistent night pain, or a history of cancer necessitate evaluation for metastatic disease. Cancers known to metastasize to bone, like breast or lung cancer, may present with back pain, requiring thorough imaging and lab work.
Infectious Causes:
Spinal infections, such as osteomyelitis or epidural abscess, are serious conditions often presenting with back pain. Risk factors include intravenous drug use or immunocompromised states. High suspicion is necessary in patients with concurrent systemic symptoms.
Cauda Equina Syndrome (CES):
CES is a neurosurgical emergency, presenting with symptoms like severe lower back pain, saddle anesthesia, and bowel or bladder dysfunction. A meticulous neurological examination, focusing on lower limb function and perineal sensation, is necessary. MRI is the preferred diagnostic tool, providing detailed images of the spinal cord and nerve roots.
Imaging and Laboratory Tests
Imaging:
Imaging choices should be guided by clinical suspicion. MRI is preferred for evaluating soft tissues, especially in suspected CES cases. For older adults, plain X-rays can reveal fractures but are limited in detecting soft tissue issues. CT scans are useful for complex cases like suspected tumors or infections, while nuclear medicine imaging may detect metastatic lesions or stress fractures.
Laboratory Tests:
Blood tests are essential in cases where red flags suggest systemic involvement. Tests like a full blood count (FBC), inflammatory markers, and bone profiles can provide critical diagnostic information. Elevated inflammatory markers may indicate infection or inflammation, while abnormal calcium levels could suggest a paraneoplastic syndrome.
Management of Non-Specific Back Pain
Once serious conditions are ruled out, management focuses on non-specific, likely musculoskeletal back pain. This involves patient education, mobilization, and appropriate pain management.
Patient Education and Mobilization:
Patients should be informed about the importance of staying active to prevent muscle stiffness and worsening pain. The role of muscle spasm in pain should be explained, and patients encouraged to maintain activity despite discomfort.
Pain Management:
The WHO pain ladder guides pain management, starting with simple analgesics like paracetamol and NSAIDs. For more severe pain, moderate opioids like codeine may be considered. The goal is to provide sufficient pain relief to facilitate mobilization and prevent the development of chronic pain.
Controversial Treatments:
The use of benzodiazepines is controversial. They are not true muscle relaxants but can reduce anxiety and distress, potentially aiding pain management. However, they should be used sparingly and for short periods. The use of gabapentin for acute back pain is also debated, as it is primarily indicated for neuropathic pain.
Chronic Pain Management
For chronic pain patients, management focuses on a multidisciplinary approach, involving pain specialists, physiotherapists, and primary care providers. The goal is to manage the physical, psychological, and social aspects of chronic pain.
Collaborative Care:
Close collaboration with primary care providers ensures consistent messaging and management plans. Pain specialists can offer additional support, especially in complex cases requiring advanced pain management techniques.
Non-Pharmacological Interventions:
Non-pharmacological interventions, such as physical therapy and cognitive-behavioral therapy (CBT), are crucial. These therapies help strengthen muscles, improve posture, and manage the psychological impacts of chronic pain.
Conclusion
In conclusion, managing back pain in the ED requires a comprehensive, systematic approach. Clinicians must prioritize ruling out serious conditions, use appropriate diagnostic tools, and provide effective pain management and patient education. Collaboration with primary care and pain specialists is essential for managing chronic pain, ensuring a holistic approach to patient care. By following these guidelines, healthcare professionals can provide compassionate, evidence-based care, leading to better patient outcomes and a more efficient emergency department.
Red flag symptoms and analgesia advice below.
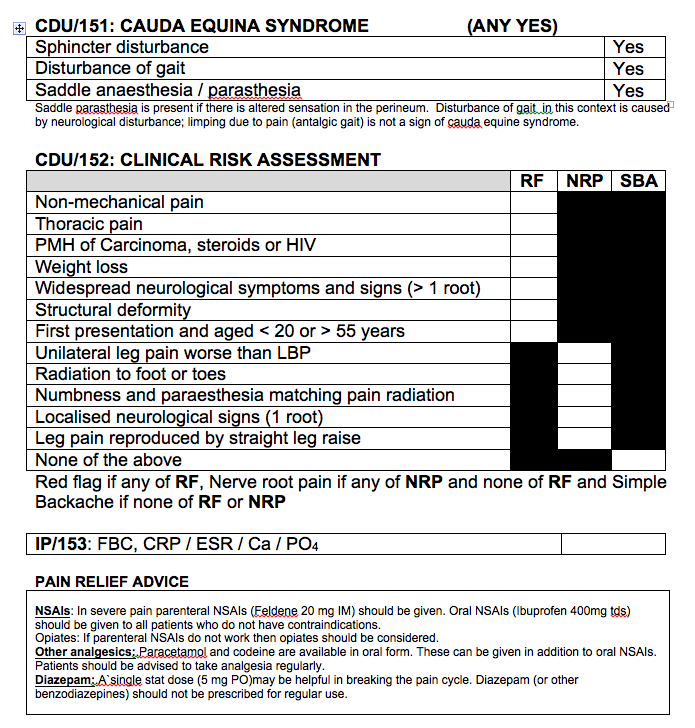

Friday May 22, 2015
Ep 47 - Barbra Backus on Risk scores in Acute Coronary syndromes
Friday May 22, 2015
Friday May 22, 2015
Barbra Backus joins Rick Body to discuss the origin, development and future of risk scores for ED patients with possible acute coronary syndromes. Two researchers at the top of their game, and authors of the HEART and MACS scores.
Wednesday May 06, 2015
Ep 46 - Intro to EM: The patient with asthma
Wednesday May 06, 2015
Wednesday May 06, 2015
Introduction
Welcome to the St. Emlyn's induction podcast recap, where we dive deep into the management of asthma in the emergency department. Asthma is a prevalent condition that emergency medical professionals encounter frequently. This blog post will provide a detailed step-by-step guide to managing patients presenting with asthma, including case presentation, assessment, treatment, and discharge planning. Whether you're a seasoned practitioner or new to emergency medicine, this guide aims to enhance your understanding and improve patient outcomes.
Case Presentation: Recognizing Severe Asthma
Imagine you're in the resuscitation room when you're alerted about an incoming patient. A 30-year-old female with a history of acute severe asthma is being brought in. She's a smoker, consuming 20 cigarettes a day, and has had a history of hospital admissions, including an ICU stay a few years ago. As she is wheeled in, you notice she is short of breath with audible wheezing. This initial presentation provides critical information for immediate action.
First Steps: Rapid Assessment and Initial Management
Upon the patient's arrival, it's crucial to make a rapid assessment. Conducting an ABC (Airway, Breathing, Circulation) assessment is essential to confirm the diagnosis and gauge the severity of the asthma attack. Given the patient's severe condition, it's vital to start treatment immediately while continuing your assessment.
Immediate Actions
- High-Flow Oxygen: Administer high-flow oxygen to improve oxygen saturation levels.
- Nebulizers: Start with 5 mg of salbutamol and 500 mcg of ipratropium bromide. Don't hesitate to administer another dose if needed.
- Listen to the Chest: A quick auscultation of the chest can help confirm the presence of wheezes and rule out other conditions like tension pneumothorax.
Understanding the Severity of Asthma
Assessing the severity of asthma is critical to guiding further treatment. The British Thoracic Society provides guidelines that classify asthma into mild, moderate, acute severe, and life-threatening categories.
Criteria for Severity
- Mild Asthma: Patients might experience mild dyspnea but can generally manage with minimal intervention.
- Moderate Asthma: Characterized by a peak flow more than 50% of predicted or best, moderate symptoms, and manageable at home with proper medication.
- Acute Severe Asthma: Marked by a peak flow below 50%, respiratory rate over 25, heart rate over 110, or an inability to complete sentences.
- Life-Threatening Asthma: Includes a peak flow less than 33%, low oxygen saturation below 92%, silent chest on auscultation, cyanosis, and signs of exhaustion.
Continuous Management: Treating Severe Asthma
In cases of severe or life-threatening asthma, continuous management and close monitoring are paramount.
Back-to-Back Nebulizers
Administering nebulizers continuously can help manage severe bronchoconstriction. Use salbutamol and ipratropium bromide back-to-back to provide relief.
Steroid Administration
Steroids play a crucial role in managing asthma by reducing inflammation. Administer oral steroids (1-2 mg/kg of prednisolone) or intravenous steroids if oral administration is not feasible.
Intravenous Bronchodilators
Consider intravenous bronchodilators like salbutamol if nebulized drugs are ineffective. Prepare IV salbutamol early to ensure it's available when needed.
Magnesium Sulfate
Magnesium sulfate can be considered in severe cases. Although recent studies suggest it might not significantly impact, it is relatively safe and may benefit a small subgroup of patients.
Advanced Interventions: When Initial Treatments Fail
If the patient's condition does not improve with initial treatments, advanced interventions may be necessary.
Critical Care Consultation
Engage with critical care colleagues early if the patient requires intensive care or ventilation. Ventilating an asthmatic patient is complex and requires experienced personnel.
Additional Therapies
- Ketamine Infusion: Ketamine can act as a bronchodilator and is used in managing severe asthma.
- CPAP: Continuous Positive Airway Pressure (CPAP) can be used in cases of severe air trapping and respiratory distress.
Importance of Senior Support
It's vital for less experienced doctors to seek senior help when managing severe asthma cases. These patients require the most experienced care available.
Discharge Planning: Ensuring Safe Transition
For patients showing improvement, careful discharge planning is essential to prevent relapse and ensure ongoing management.
Criteria for Discharge
- Stability: Ensure the patient is stable for at least 6-8 hours after initial treatment.
- Follow-Up: Arrange follow-up with a general practitioner or asthma nurse within a few days.
- Medication Review: Ensure the patient has access to their inhalers and understands their use.
- Safety Netting: Advise the patient to return if symptoms worsen, even if they are already on their way home.
Safety Measures
Natalie May from St. Emlyn's emphasizes the importance of advising patients to return if they have any concerns, even after leaving the hospital. Ensuring patients have their therapy and understand their treatment plan is crucial for safe discharge.
Conclusion: Recap and Key Takeaways
In summary, managing asthma in the emergency department requires a systematic approach:
- Rapid Assessment: Quickly assess the severity using ABC and confirm the diagnosis.
- Immediate Treatment: Administer high-flow oxygen and nebulizers without delay.
- Continuous Management: Use back-to-back nebulizers, steroids, and consider IV bronchodilators and magnesium sulfate.
- Advanced Interventions: Engage critical care and consider additional therapies like ketamine and CPAP.
- Discharge Planning: Ensure the patient is stable, arrange follow-up, review medications, and provide safety netting advice.
Asthma management in emergency settings is challenging but manageable with the right approach and timely interventions. Always prioritize the patient's safety and seek senior support when needed.
Further Resources
For more detailed information, refer to the British Thoracic Society guidelines and explore additional induction podcasts available on iTunes. Staying updated with the latest research and best practices is essential for improving patient outcomes in asthma management.
References
- British Thoracic Society Guidelines
- St. Emlyn's Induction Podcasts
- Recent Studies on Magnesium Sulfate in Asthma Management
Keywords
- Asthma management
- Emergency department
- Severe asthma
- Life-threatening asthma
- High-flow oxygen
- Nebulizers
- Salbutamol
- Ipratropium bromide
- Steroids in asthma
- Intravenous bronchodilators
- Magnesium sulfate
- Critical care in asthma
- CPAP in asthma
- Ketamine infusion
- Asthma discharge planning
By following these guidelines and staying informed, healthcare professionals can effectively manage asthma in emergency settings, ensuring the best possible outcomes for their patients.
Recognizing and Managing Severe Asthma in the Emergency Department: A Detailed Guide
Asthma is a common condition frequently encountered in emergency departments. Managing patients presenting with asthma, particularly those with severe symptoms, requires a systematic and prompt approach. This guide will focus on the initial assessment and management steps for a patient presenting with severe asthma in the emergency department, providing detailed insights into immediate actions and the rationale behind them.
Case Presentation: Recognizing Severe Asthma
Consider a typical scenario in the resuscitation room. You receive an alert about a 30-year-old female with a history of acute severe asthma. This patient, a smoker who consumes 20 cigarettes a day, has previously been admitted to the ICU for asthma-related issues. She is brought in, visibly short of breath and with an audible wheeze.
This initial presentation is critical for immediate action. Recognizing the signs of severe asthma and understanding the patient's history sets the stage for effective management.
Initial Management: Rapid Assessment and Treatment
Upon the patient's arrival, a rapid assessment is essential. Conducting an ABC (Airway, Breathing, Circulation) assessment helps confirm the diagnosis and determine the severity of the asthma attack. Given the patient's severe condition, simultaneous assessment and treatment are necessary.
Immediate Actions
-
Administer High-Flow Oxygen: The first step is to administer high-flow oxygen. This intervention aims to improve the patient's oxygen saturation levels, which is crucial for stabilizing their condition.
-
Start Nebulizers: Administer a combination of 5 mg of salbutamol and 500 mcg of ipratropium bromide. These medications help relax the bronchial muscles and reduce bronchospasm. If the patient remains symptomatic, additional doses can be given without hesitation.
-
Listen to the Chest: A quick auscultation of the chest can confirm the presence of wheezes and rule out other conditions, such as a tension pneumothorax. This step ensures that the treatment plan is appropriate and targeted.
Understanding Asthma Severity
Assessing the severity of asthma is crucial for guiding treatment decisions. The British Thoracic Society's guidelines classify asthma into mild, moderate, acute severe, and life-threatening categories based on specific clinical criteria.
Severity Criteria
-
Mild Asthma: Patients with mild asthma may experience mild dyspnea and can usually manage with minimal intervention.
-
Moderate Asthma: This category is characterized by a peak flow more than 50% of predicted or best, moderate symptoms, and manageable with proper medication at home.
-
Acute Severe Asthma: Patients in this category have a peak flow below 50%, respiratory rate over 25, heart rate over 110, or an inability to complete sentences. Immediate and aggressive treatment is required.
-
Life-Threatening Asthma: This is marked by a peak flow less than 33%, low oxygen saturation below 92%, silent chest on auscultation, cyanosis, and signs of exhaustion. These patients require urgent and intensive intervention.
Continuous Management: Treating Severe Asthma
For patients with severe or life-threatening asthma, continuous management and close monitoring are essential.
Back-to-Back Nebulizers
Administering nebulizers continuously can help manage severe bronchoconstriction. Salbutamol and ipratropium bromide should be given back-to-back to provide maximum relief.
Steroid Administration
Steroids are crucial in managing asthma by reducing inflammation. Administer oral steroids, such as 1-2 mg/kg of prednisolone, or intravenous steroids if oral administration is not feasible. While steroids do not provide immediate relief, they help reduce the underlying inflammation and prevent future exacerbations.
Intravenous Bronchodilators
Consider intravenous bronchodilators like salbutamol if nebulized drugs are ineffective. Prepare IV salbutamol early to ensure it is available when needed.
Magnesium Sulfate
Magnesium sulfate can be considered in severe cases. Although recent studies suggest it might not significantly impact, it is relatively safe and may benefit a small subgroup of patients. However, it should not delay other critical treatments.
Advanced Interventions: When Initial Treatments Fail
If the patient's condition does not improve with initial treatments, advanced interventions may be necessary.
Critical Care Consultation
Engage with critical care colleagues early if the patient requires intensive care or ventilation. Ventilating an asthmatic patient is complex and requires experienced personnel.
Additional Therapies
-
Ketamine Infusion: Ketamine can act as a bronchodilator and is used in managing severe asthma.
-
CPAP: Continuous Positive Airway Pressure (CPAP) can be used in cases of severe air trapping and respiratory distress.
Importance of Senior Support
It is vital for less experienced doctors to seek senior help when managing severe asthma cases. These patients require the most experienced care available.
Discharge Planning: Ensuring Safe Transition
For patients showing improvement, careful discharge planning is essential to prevent relapse and ensure ongoing management.
Criteria for Discharge
-
Stability: Ensure the patient is stable for at least 6-8 hours after initial treatment.
-
Follow-Up: Arrange follow-up with a general practitioner or asthma nurse within a few days.
-
Medication Review: Ensure the patient has access to their inhalers and understands their use.
-
Safety Netting: Advise the patient to return if symptoms worsen, even if they are already on their way home.
Safety Measures
Natalie May from St. Emlyn's emphasizes the importance of advising patients to return if they have any concerns, even after leaving the hospital. Ensuring patients have their therapy and understand their treatment plan is crucial for safe discharge.
Conclusion: Recap and Key Takeaways
In summary, managing asthma in the emergency department requires a systematic approach:
-
Rapid Assessment: Quickly assess the severity using ABC and confirm the diagnosis.
-
Immediate Treatment: Administer high-flow oxygen and nebulizers without delay.
-
Continuous Management: Use back-to-back nebulizers, steroids, and consider IV bronchodilators and magnesium sulfate.
-
Advanced Interventions: Engage critical care and consider additional therapies like ketamine and CPAP.
-
Discharge Planning: Ensure the patient is stable, arrange follow-up, review medications, and provide safety netting advice.
Asthma management in emergency settings is challenging but manageable with the right approach and timely interventions. Always prioritize the patient's safety and seek senior support when needed.
By following these guidelines and staying informed, healthcare professionals can effectively manage asthma in emergency settings, ensuring the best possible outcomes for their patients.
First Command: Initial Management of Severe Asthma in the Emergency Department
Asthma is a common, chronic respiratory condition that often presents acutely in emergency departments. Managing a severe asthma attack requires immediate and decisive action to prevent life-threatening complications. This guide will walk you through the first command in the management of severe asthma: recognizing the severity of the condition and initiating appropriate treatment promptly.
Case Scenario
Picture yourself in the resuscitation room when you receive an alert about a patient en route to the hospital. The patient is a 30-year-old female with a history of acute severe asthma. She is a 20-a-day smoker and has had previous hospital admissions, including a stay in the Intensive Care Unit (ICU) a few years ago. Upon her arrival, she is visibly short of breath with an audible wheeze.
Immediate Assessment and Treatment
Upon the patient's arrival, it is critical to make a rapid assessment and initiate treatment simultaneously. The goals are to confirm the diagnosis, assess the severity of the asthma attack, and begin interventions that can stabilize the patient.
Rapid Assessment: ABC Approach
-
Airway: Ensure the airway is clear. Asthma patients typically do not have airway obstructions, but it is crucial to check for any foreign bodies or swelling that might complicate the condition.
-
Breathing: Assess the patient's breathing. Look for signs of respiratory distress, such as rapid breathing, use of accessory muscles, and the presence of wheezing. Measure oxygen saturation using a pulse oximeter.
-
Circulation: Check the patient's heart rate and blood pressure. Asthma can cause tachycardia and hypertension due to the stress of breathing difficulties.
Initial Actions
-
Administer High-Flow Oxygen: The first and most crucial step is to administer high-flow oxygen. This intervention aims to improve the patient's oxygen saturation levels. Use a non-rebreather mask to deliver a high concentration of oxygen (usually 15 liters per minute).
-
Start Nebulizers: Administer bronchodilators through a nebulizer. Begin with 5 mg of salbutamol and 500 mcg of ipratropium bromide. These medications help to relax the bronchial muscles and reduce bronchospasm, facilitating easier breathing. If the patient remains symptomatic, additional doses can be administered without hesitation.
-
Listen to the Chest: Perform a quick auscultation of the chest to confirm the presence of wheezes and rule out other conditions such as a tension pneumothorax. The presence of bilateral wheezing supports the diagnosis of an asthma exacerbation.
Understanding Asthma Severity
Assessing the severity of the asthma attack is essential for guiding treatment decisions. The British Thoracic Society classifies asthma into mild, moderate, acute severe, and life-threatening categories based on specific clinical criteria.
Severity Criteria
-
Mild Asthma: Patients with mild asthma may experience mild dyspnea and can usually manage with minimal intervention.
-
Moderate Asthma: Characterized by a peak flow more than 50% of predicted or best, moderate symptoms, and manageable with proper medication at home.
-
Acute Severe Asthma: Patients in this category have a peak flow below 50%, respiratory rate over 25, heart rate over 110, or an inability to complete sentences. Immediate and aggressive treatment is required.
-
Life-Threatening Asthma: Marked by a peak flow less than 33%, low oxygen saturation below 92%, silent chest on auscultation, cyanosis, and signs of exhaustion. These patients require urgent and intensive intervention.
Continuous Management: Treating Severe Asthma
For patients with severe or life-threatening asthma, continuous management and close monitoring are essential.
Back-to-Back Nebulizers
Administering nebulizers continuously can help manage severe bronchoconstriction. Salbutamol and ipratropium bromide should be given back-to-back to provide maximum relief. This approach ensures that the bronchodilators maintain their effect, reducing airway resistance and improving airflow.
Steroid Administration
Steroids play a crucial role in managing asthma by reducing inflammation. Administer oral steroids, such as 1-2 mg/kg of prednisolone, or intravenous steroids if oral administration is not feasible. While steroids do not provide immediate relief, they help reduce the underlying inflammation and prevent future exacerbations.
Intravenous Bronchodilators
Consider intravenous bronchodilators like salbutamol if nebulized drugs are ineffective. Prepare IV salbutamol early to ensure it is available when needed. Intravenous administration allows the medication to reach the target sites quickly, providing more effective relief in severe cases.
Magnesium Sulfate
Magnesium sulfate can be considered in severe cases. Although recent studies suggest it might not significantly impact, it is relatively safe and may benefit a small subgroup of patients. However, it should not delay other critical treatments.
Advanced Interventions: When Initial Treatments Fail
If the patient's condition does not improve with initial treatments, advanced interventions may be necessary.
Critical Care Consultation
Engage with critical care colleagues early if the patient requires intensive care or ventilation. Ventilating an asthmatic patient is complex and requires experienced personnel. Early involvement of critical care can facilitate the management of severe cases and improve patient outcomes.
Additional Therapies
-
Ketamine Infusion: Ketamine can act as a bronchodilator and is used in managing severe asthma. It provides sedation and bronchodilation, which can be beneficial in severe cases.
-
CPAP: Continuous Positive Airway Pressure (CPAP) can be used in cases of severe air trapping and respiratory distress. It helps to keep the airways open and reduce the work of breathing.
Importance of Senior Support
It is vital for less experienced doctors to seek senior help when managing severe asthma cases. These patients require the most experienced care available. Senior clinicians can provide guidance on advanced therapies and ensure that all possible interventions are considered.
Conclusion: Recap and Key Takeaways
Managing severe asthma in the emergency department requires a systematic and prompt approach:
-
Rapid Assessment: Quickly assess the severity using the ABC approach and confirm the diagnosis.
-
Immediate Treatment: Administer high-flow oxygen and nebulizers without delay.
-
Continuous Management: Use back-to-back nebulizers, steroids, and consider intravenous bronchodilators and magnesium sulfate.
-
Advanced Interventions: Engage critical care and consider additional therapies like ketamine and CPAP.
Asthma management in emergency settings is challenging but manageable with the right approach and timely interventions. Always prioritize the patient's safety and seek senior support when needed.
By following these guidelines, healthcare professionals can effectively manage severe asthma in emergency settings, ensuring the best possible outcomes for their patients.

Monday Apr 27, 2015
Ep 45 - Top 10 trauma papers 2014-2015.
Monday Apr 27, 2015
Monday Apr 27, 2015
A first podcast with Simon Laing from the RCEMFOAMed team. We look back at influential trauma related papers from 2014-2015.

Saturday Apr 18, 2015
Ep 44 - Tim Draycott on Obstetric Trauma (LTC 2014)
Saturday Apr 18, 2015
Saturday Apr 18, 2015
Iain interviews the wonderful Tim Draycott on the management of the Obstetric patient with trauma.Tim is a consultant Obstetrician from Bristol and is a great speaker on this rather terrifying topic!

Thursday Mar 26, 2015
Ep 43 - APLS 2015 updates for the management of the serious injured child
Thursday Mar 26, 2015
Thursday Mar 26, 2015

A short podcast updating the UK Advanced Paediatric Life Support (APLS) course guidelines for the management of trauma in children.
Don't forget to read the blog post here. APLS Updates: New kids on the block,
vb
S
Sunday Mar 22, 2015
Ep 42 - Paediatric Major Trauma with Ross Fisher (LTC 2014)
Sunday Mar 22, 2015
Sunday Mar 22, 2015
Title: Rethinking Pediatric Trauma: Insights from the London Trauma Conference
Welcome to another insightful post from St Emlyns, where we dive into the latest discussions and research in emergency medicine. In this post, we recap a conversation with Rosfisher, a pediatric surgeon from Sheffield, who recently presented at the London Trauma Conference. Rosfisher shared his perspectives on pediatric trauma management, the challenges of research in this field, and the art of effective presentation. Let's explore these critical topics and their implications for emergency care.
Pediatric Trauma: A Unique Challenge
Pediatric trauma is an infrequent yet crucial area in emergency medicine, necessitating a distinct approach. Rosfisher emphasized that children are not simply "small adults." This fundamental concept underlines the need for specialized knowledge and skills when managing pediatric trauma. Despite the rarity of severe pediatric trauma cases, healthcare professionals must understand that children's anatomical, physiological, and pathological differences require tailored treatment strategies.
Understanding the Differences
One of the key points Rosfisher highlighted is the unique nature of pediatric anatomy and physiology. Unlike adults, children have different injury patterns, and their bodies respond differently to trauma. This distinction is crucial for emergency physicians, pediatric surgeons, and anesthetists, who must adjust their standard protocols to suit pediatric needs. The importance of recognizing these differences cannot be overstated, as it directly impacts the outcomes of pediatric trauma cases.
The Debate on FAST Scanning in Pediatric Trauma
A significant portion of Rosfisher's discussion focused on the use of Focused Assessment with Sonography for Trauma (FAST) in pediatric cases. While FAST scanning is a well-established practice in adult trauma, its efficacy in pediatric patients remains controversial. Rosfisher pointed out the lack of robust evidence supporting the reliability of FAST scans in children, citing a 50% sensitivity and specificity rate—equivalent to flipping a coin.
Limitations and Concerns
The concerns surrounding FAST scanning in pediatric trauma revolve around its diagnostic accuracy and the subsequent decision-making process. Rosfisher noted that even if healthcare professionals are skilled in using FAST scans on adults, this expertise does not necessarily translate to pediatric patients. The anatomical and physiological differences mean that the interpretation of FAST scans in children is more complex and less reliable. As a result, the decisions based on these scans carry a high risk of error.
The Role of CT Scans
In light of the limitations of FAST scanning, Rosfisher advocated for the use of computed tomography (CT) scans for pediatric blunt abdominal trauma. He referenced guidelines from the Royal College of Radiology, which recommend CT scans as the gold standard for imaging in these cases. The higher accuracy and reliability of CT scans make them a preferable option, providing clearer insights into the child's condition and guiding appropriate treatment.
Challenges in Pediatric Trauma Research
Pediatric trauma research is significantly underrepresented compared to adult trauma research. Rosfisher highlighted the stark contrast in research volume, with pediatric studies comprising less than half a percent of the total trauma research. This disparity poses a considerable challenge, as the lack of data hampers the development of evidence-based practices in pediatric trauma care.
Barriers to Research
Several factors contribute to the limited research in pediatric trauma. One major issue is the misconception that pediatric trauma is simply a scaled-down version of adult trauma. This oversimplification overlooks the complexities unique to children and the necessity for dedicated research in this area. Additionally, the relatively low incidence of pediatric trauma cases can make it difficult to conduct large-scale studies, further limiting the available data.
Opportunities for Growth
Despite these challenges, there is significant potential for growth in pediatric trauma research. The emergence of pediatric emergency medicine as a specialized field offers new avenues for research and development. Networks like PERUKI (Pediatric Emergency Research in the UK and Ireland) provide platforms for collaboration and innovation, encouraging more healthcare professionals to engage in pediatric trauma research.
Enhancing Presentation Skills in Medicine
Beyond his expertise in pediatric trauma, Rosfisher is passionate about improving presentation skills within the medical community. He argues that the way information is presented can significantly impact its retention and application. Many presentations, despite being rich in content, fail to leave a lasting impression due to poor delivery.
The Importance of Storytelling
Rosfisher advocates for incorporating storytelling into presentations. A well-structured narrative helps audiences follow the flow of information and retain key points. He uses the concept of an "arc of a story," similar to a plot in a film or book, to structure his talks. This approach ensures that the audience remains engaged and can easily recall the main message.
Practical Tips for Effective Presentations
For those looking to improve their presentation skills, Rosfisher offers several practical tips:
-
Know Your Content: Before delivering a talk, ensure you have a deep understanding of the subject matter. This foundation is essential for building a coherent and compelling presentation.
-
Elevator Pitch: Condense your talk into a brief "elevator pitch." If you can explain the essence of your presentation in 30 seconds, you are more likely to deliver a clear and focused message.
-
Audience Awareness: Tailor your presentation to your audience's needs and knowledge level. Understanding where your audience starts and where you want them to end up helps in crafting a relevant and impactful message.
-
Visual Aids: Use visuals to support your narrative. Rather than cluttering slides with text, use images and simple graphics that complement your spoken words and enhance understanding.
-
Consistency and Repetition: Start and end your presentation with the same message or visual cue. This technique reinforces the key takeaway and helps embed it in the audience's memory.
Case Study: Effective Use of Visual Aids
During his presentation at the London Trauma Conference, Rosfisher used several effective visual aids. He started and ended with the same video, challenging the audience to rethink their perspectives on pediatric trauma. He also employed a memorable device using the numbers 73 and 37, referencing the popular TV show "The Big Bang Theory." This consistent thread helped tie together various statistics and made the information more memorable for the audience.
Conclusion: A Call to Action in Pediatric Trauma
The insights shared by Rosfisher at the London Trauma Conference underscore the need for a nuanced approach to pediatric trauma. Recognizing that children are not small adults is a fundamental step in improving care and outcomes in this field. The discussions around the use of FAST scanning highlight the importance of evidence-based practices, while the challenges in pediatric trauma research call for greater investment and focus.
As healthcare professionals, it's crucial to continue exploring new methods and technologies, like CT scans, that can enhance diagnostic accuracy and treatment efficacy in pediatric cases. Moreover, by honing our presentation skills, we can ensure that vital knowledge and insights are effectively communicated, leading to better understanding and implementation of best practices.
In conclusion, pediatric trauma care requires a specialized approach, and the field offers numerous opportunities for research and innovation. We encourage our readers to engage with networks like PERUKI, contribute to research efforts, and continuously refine their skills, both in clinical practice and communication. Together, we can make significant strides in improving the care and outcomes for our youngest and most vulnerable patients.
Stay tuned for more insights and discussions from the St Emlyns blog, where we continue to explore the latest in emergency medicine and critical care. Don't forget to subscribe and follow us on social media for updates on our latest posts and podcasts.
Title: Rethinking Pediatric Trauma: Key Insights from the London Trauma Conference
In a recent discussion at the London Trauma Conference, Rosfisher, a pediatric surgeon from Sheffield, provided valuable insights into pediatric trauma care, the challenges of research in this field, and effective presentation techniques. This summary captures the key points from his presentations and discussions.
Pediatric Trauma: Understanding the Differences
Pediatric trauma presents unique challenges in emergency medicine. Rosfisher emphasized that children are not merely "small adults," a common misconception that can lead to inadequate care. The distinct anatomical, physiological, and pathological characteristics of children necessitate specialized approaches to treatment. Recognizing these differences is crucial for healthcare professionals, including emergency physicians, pediatric surgeons, and anesthetists, who must adjust their standard protocols accordingly.
The Controversy Around FAST Scanning
A significant portion of the discussion focused on the use of Focused Assessment with Sonography for Trauma (FAST) in pediatric cases. While FAST scanning is a well-established diagnostic tool in adult trauma, its efficacy in children is debatable. Rosfisher highlighted the lack of strong evidence supporting the reliability of FAST scans in pediatric trauma, citing a 50% sensitivity and specificity rate. This level of accuracy is akin to chance, making it a less reliable diagnostic tool for children.
The concern with FAST scanning lies not only in its accuracy but also in the potential consequences of basing clinical decisions on these results. Even experienced practitioners may struggle with interpreting FAST scans in children due to their distinct anatomical differences. As a result, there is a significant risk of incorrect decision-making. Rosfisher advocates for the use of computed tomography (CT) scans instead, as they offer more accurate and reliable imaging for pediatric blunt abdominal trauma. This recommendation aligns with guidelines from the Royal College of Radiology, which consider CT scans the gold standard in these cases.
Challenges in Pediatric Trauma Research
Research in pediatric trauma is significantly underrepresented compared to adult trauma research. Rosfisher pointed out that pediatric studies account for less than half a percent of all trauma research. This paucity of data presents a major challenge in developing evidence-based practices for pediatric trauma care. Several factors contribute to this lack of research, including the misconception that pediatric trauma is simply a scaled-down version of adult trauma and the relatively low incidence of severe pediatric trauma cases.
Despite these challenges, there is significant potential for growth in pediatric trauma research. The rise of pediatric emergency medicine as a specialized field offers new opportunities for research and innovation. Networks like PERUKI (Pediatric Emergency Research in the UK and Ireland) are fostering collaboration and encouraging more research in this area. Rosfisher emphasized the importance of starting with simple audit projects to assess current practices and gradually build a more comprehensive understanding of pediatric trauma care.
Improving Presentation Skills in Medicine
Beyond his expertise in pediatric trauma, Rosfisher is passionate about improving presentation skills within the medical community. He argues that the effective presentation of information is crucial for ensuring that important insights and knowledge are retained and applied. Often, the wisdom shared during medical presentations is lost due to poor delivery.
Rosfisher advocates for a storytelling approach in presentations. A well-structured narrative helps engage the audience and makes the information more memorable. He uses the concept of an "arc of a story," which involves structuring a presentation with a clear beginning, middle, and end, much like a film or book. This method helps the audience follow the flow of information and retain key points.
Practical Tips for Effective Presentations
Rosfisher offers several practical tips for improving presentation skills:
-
Master Your Content: Ensure a deep understanding of the subject matter. A technique like the "elevator pitch" can help distill the essence of a presentation into a concise summary, ensuring clarity and focus.
-
Audience Awareness: Tailor the presentation to the audience's knowledge level and interests. Understanding where the audience starts and where they should be by the end of the presentation is key to crafting an effective message.
-
Use of Visual Aids: Visuals should support the narrative rather than clutter the presentation with text. Images and simple graphics can enhance understanding and retention.
-
Consistency and Repetition: Using consistent themes and repeating key messages can reinforce the main points. For example, starting and ending a presentation with the same message or visual cue can help embed the information in the audience's memory.
Conclusion: A Call to Action in Pediatric Trauma
Rosfisher's insights highlight the need for a nuanced and specialized approach to pediatric trauma care. Recognizing the fundamental differences between children and adults is essential for providing appropriate treatment and improving outcomes. The debate around FAST scanning underscores the importance of evidence-based practices, while the challenges in pediatric trauma research call for increased focus and investment.
For healthcare professionals, engaging with research networks like PERUKI and contributing to pediatric trauma research are crucial steps toward advancing the field. Additionally, improving presentation skills can enhance the dissemination and retention of critical knowledge, leading to better clinical practices.
As we continue to explore and improve pediatric trauma care, we encourage our readers to stay engaged with ongoing research and professional development. Together, we can make significant strides in providing the best care for our youngest patients. Stay tuned for more insights and discussions from St Emlyns, where we continue to explore the latest in emergency medicine and critical care.
Sunday Mar 15, 2015
Ep 41 - Is trauma an elite sport? with Tom Evens (LTC 2014)
Sunday Mar 15, 2015
Sunday Mar 15, 2015
High-Performance in Trauma Care: Lessons from Elite Sports Coaching
Welcome to the St Emlyns blog! Today, we're diving into an insightful discussion from the recent London Trauma Conference, where Dr. Tom Evans shared his unique experiences and lessons learned from working with the British rowing team as a coach. Dr. Evans, a post-CCT doctor in emergency medicine and former Sydney HEMS doctor, offers a fascinating perspective on high-performance culture in trauma care, drawing parallels with elite sports coaching.
The Challenge of High Performance in Trauma Care
In trauma care, the term "world-class" is often used to describe top-tier performance. However, as Dr. Evans points out, this concept can be misleading. Unlike athletes who prepare for specific, well-defined events, emergency medicine professionals face an unpredictable array of cases daily. Thus, instead of striving to be "world-class," a more practical and applicable goal is to focus on achieving "high performance."
High performance is not an end result but a continuous process. It involves creating a culture where every team member is committed to doing even the smallest tasks as well as possible. This mindset shift from an outcome-based to a process-oriented approach is crucial for trauma teams, as it emphasizes excellence in everyday practice rather than sporadic peak performances.
High-Performance Culture: Key Components
-
Shared Mental Models: One of the key aspects of high-performance teams, both in sports and healthcare, is the creation of shared mental models. In coaching, athletes need a clear understanding of what their performance should look like. This clarity helps them execute their skills effectively under pressure. Similarly, in trauma care, standard operating procedures (SOPs) help create a shared understanding among team members. This reduces cognitive load and allows team members to anticipate actions and outcomes, leading to better coordinated and more effective care.
-
Simulation and Visualization: Dr. Evans emphasizes the importance of simulation and visualization in preparing for high-stress situations. Just as athletes use these techniques to mentally rehearse their performances, healthcare professionals can use simulation training to test and refine their responses to various scenarios. High-pressure simulations are particularly valuable as they help teams assess their readiness and make necessary adjustments to their mental models.
-
Marginal Gains and the Basics: The concept of marginal gains—small incremental improvements—is widely recognized in elite sports. However, Dr. Evans cautions against focusing solely on these gains without first mastering the basics. In trauma care, the foundational elements such as knowledge, systems, and debriefing must be solid. Marginal gains can only be beneficial when the team operates consistently at a high level. Therefore, trauma teams should prioritize getting the basics right before seeking minor improvements.
Training vs. Coaching: A Crucial Distinction
A critical insight from Dr. Evans is the difference between training and coaching. In medical education, training often focuses on imparting knowledge and passing exams. However, coaching is about enhancing performance and preparing individuals for real-world challenges. Coaches are invested in their athletes' performance outcomes and see success as tied directly to their athletes' achievements. This personalized and performance-driven approach contrasts with the often fragmented nature of medical training, where trainees rotate through multiple trainers and institutions.
Dr. Evans argues for a coaching approach in medical training. This would involve more personalized guidance and a focus on developing the skills and mindset needed for long-term success in the field. Such an approach could better prepare trainees for the unpredictable and high-stakes nature of trauma care.
Implementing High-Performance Strategies in Trauma Teams
To implement a high-performance culture in trauma care, several strategies can be adopted:
-
Institutional Support and Investment: High-performance training requires time and resources. Hospitals and healthcare institutions must prioritize training and development, even if it means adjusting schedules or reducing clinical productivity temporarily. This investment is crucial for cultivating a culture of continuous improvement and excellence.
-
Team-Based Training and Debriefing: Multi-specialty training and team-based exercises can help build a cohesive unit capable of high performance. Regular debriefing sessions after simulations and real cases are also essential. They provide opportunities for reflection, learning, and refinement of processes.
-
Focus on Human Factors: Understanding and optimizing human factors—such as communication, teamwork, and decision-making under pressure—is vital. Incorporating these elements into training and everyday practice can significantly enhance team performance.
-
Continuous Learning and Adaptation: The landscape of trauma care is constantly evolving, with new technologies and methodologies emerging. A high-performance team must be committed to continuous learning and adaptation, staying abreast of the latest developments and integrating them into practice.
Conclusion: A Call to Action for Trauma Teams
Dr. Tom Evans' insights offer a valuable perspective on achieving high performance in trauma care. By adopting strategies from elite sports coaching, trauma teams can cultivate a culture of excellence that prioritizes process, preparation, and continuous improvement. The shift from an outcome-focused to a process-oriented mindset, coupled with robust training and support, can lead to significant advancements in patient care and team effectiveness.
At St Emlyn's, we are committed to exploring innovative approaches to medical education and practice. We encourage our readers to consider how these high-performance principles can be integrated into their teams and institutions. Let's strive for excellence not just in the big moments but in every aspect of our work.
For more insights and discussions on trauma care, emergency medicine, and high-performance culture, stay tuned to the St Emlyns blog. Your feedback and experiences are always welcome, so feel free to share your thoughts in the comments below.

Friday Feb 27, 2015
Ep 40 - Opiate overdose in the ED
Friday Feb 27, 2015
Friday Feb 27, 2015
Managing Opiate Overdoses: Key Insights from St Emlyns
Opiate overdoses are a common and critical issue faced in emergency departments, especially in urban areas with prevalent drug use. This guide, based on insights from Dr. Simon Carley and Dr. Iain Beardsell, provides an in-depth look at recognizing, treating, and managing opiate overdoses, including potential complications and best practices for patient care.
Recognizing Opiate Overdoses
Patients present with opiate overdoses either accidentally or intentionally, including drug addicts, elderly patients overdosing on prescriptions, and those attempting self-harm. Recognizing an overdose involves identifying key symptoms:
- Depressed Level of Consciousness: Patients may appear lethargic or unresponsive.
- Respiratory Depression: A significantly reduced breathing rate.
- Myosis: Pinpoint pupils that are unresponsive to light.
- Cardiovascular Effects: In severe cases, patients may exhibit hypotension or bradycardia.
Initial Assessment and ABC Protocol
In cases of suspected opiate overdose, the initial assessment should follow the ABC (Airway, Breathing, Circulation) protocol:
- Airway: Ensure the airway is open and clear.
- Breathing: Assess and support breathing and ventilation as necessary.
- Circulation: Check for adequate blood pressure and oxygen saturation. Establish IV access for medication administration.
Administering Naloxone
Naloxone, an opiate antagonist, is the primary antidote for opiate overdoses. However, its administration must be cautious and titrated to avoid complications like acute withdrawal or revealing underlying conditions, such as stimulant overdoses.
Methods of Administration
- Intravenous (IV): Offers rapid onset, but should be administered in small aliquots (e.g., 100 micrograms) to prevent abrupt awakening and associated risks.
- Intramuscular (IM): Useful when IV access is challenging, though it has variable absorption rates.
- Intranasal (IN): Effective, especially in patients with adequate spontaneous respiration.
- Nebulized Naloxone: Useful for patients who are breathing but not fully responsive, allowing gradual titration.
Managing Long-Acting Opiates
Patients who have ingested long-acting opiates, such as methadone, require careful monitoring. Continuous naloxone infusion may be necessary to prevent re-sedation. The infusion rate should typically be two-thirds of the total dose needed to achieve the initial response.
Importance of Monitoring
Patients should be placed in a setting where continuous monitoring of ventilation can be performed. Suitable locations include:
- High Dependency Unit (HDU): For intensive monitoring.
- Acute Medical Unit (AMU): For stable patients needing continuous observation.
Advanced Monitoring Techniques
End-tidal CO2 monitoring can provide a continuous assessment of respiratory status, especially when high-flow oxygen is used, which can mask hypoventilation.
Addressing Concurrent Conditions
Opiate overdoses often coexist with other medical or substance-related conditions. Be vigilant for:
- Rhabdomyolysis: Caused by prolonged immobility, leading to muscle breakdown.
- Compartment Syndrome: Particularly in patients found unconscious for extended periods.
- Mixed Overdoses: Patients may also have ingested other substances like stimulants or tricyclic antidepressants, complicating treatment.
Psychosocial Considerations and Follow-Up
Patients presenting with opiate overdoses often have complex psychosocial needs. It is crucial to address these issues, including:
- Mental Health Assessment: Evaluate for deliberate self-harm and provide psychiatric support.
- Drug and Alcohol Services: Connect patients with support services for addiction.
- Homelessness Support: Involve homeless outreach teams as necessary.
Handling Recurrent Overdoses
It's not uncommon for patients to return with repeated overdoses, reflecting the chronic nature of addiction. While frustrating, healthcare providers must consistently offer support and care, recognizing that patients have autonomy in their choices.
Controversies and Emerging Practices
Recent case reports suggest potential benefits in ventilating hypercapnic, acidotic patients before administering naloxone to avoid complications like flash pulmonary edema or dysrhythmias. However, this practice remains controversial and requires careful risk-benefit analysis.
Case Study Insight
A notable case involved a pregnant patient with an opiate overdose who also had ingested cocaine and tricyclic antidepressants. Administering a high dose of naloxone precipitated severe withdrawal and unmasked the effects of other substances, leading to a critical situation. This highlights the importance of a controlled and gradual approach to naloxone administration.
Conclusion
Effective management of opiate overdoses in the emergency department requires a nuanced approach. This includes recognizing the signs, following the ABC protocol, and carefully administering naloxone. Continuous monitoring, addressing underlying conditions, and providing psychosocial support are crucial for comprehensive care. Stay informed on emerging practices and best practices to enhance patient outcomes. For more detailed guidelines and updates, follow the St Emlyns blog and join our discussions on emergency medicine best practices.
