
1.3M
Downloads
272
Episodes
A UK based Emergency Medicine podcast for anyone who works in emergency care. The St Emlyn ’s team are all passionate educators and clinicians who strive to bring you the best evidence based education. Our four pillars of learning are evidence-based medicine, clinical excellence, personal development and the philosophical overview of emergency care. We have a strong academic faculty and reputation for high quality education presented through multimedia platforms and articles. St Emlyn’s is a name given to a fictionalised emergency care system. This online clinical space is designed to allow clinical care to be discussed without compromising the safety or confidentiality of patients or clinicians.
Episodes
Thursday May 20, 2021
Ep 190 - Adult Congenital Heart Disease in the ED: Part 1
Thursday May 20, 2021
Thursday May 20, 2021
This is the first in a two part podcast series discussing Adult Congenital Heart Disease (ACHD) and how these patients may present to the Emergency Department (ED). Dr Sam Fitzsimmons, our guest on the podcast, is a Consultant in Adult Congenital Heart Disease at University Hospital Southampton. There is more information in this blog post.
Look out for Part 2, which will be released next week, where we discuss Eisenmenger Syndrome, Transposition of the Great Arteries and Coarctation of the Aorta.
Background
With advances in paediatric cardiac surgery, more and more patients with complex congenital heart disease are surviving to adulthood: in the 1950s you might expect a survival rate of about 10%, whereas now this is more like 85%. In fact, there are more patients in the adult congenital heart disease population than there are in the paediatric one (with 2.3 million adults vs 1.9 million children in Europe).
Many patients with Adult Congenital Heart Disease are young and able to live a relatively normal life. This means that they can travel and take part in just the same sort of activities as those without ACHD. They may well turn up in your Emergency Department one day, regardless of whether you are a tertiary centre or a district general hospital (DGH).
They are experts, and know their disease well, but this does not abstain you from a responsibility to know about them too! When these patients become unwell, they can go downhill very fast and you may not have the chance to discuss with them their exact lesion and its management.
The anatomy and physiology of these patients is abnormal, so they may present in atypical ways, and may not respond to usual medical interventions: in fact, some of our usual treatments may even be harmful.
However, starting with our usual 'ABC' approach is by far the best way to go, whilst gathering more information and contacting their specialist centre. Many patients will have their last clinic letter and ECG with them (which will also have the direct dial number of their specialist). And if they, or their relative, say there is something wrong you must believe them and do all you can to make sure they are fully investigated.
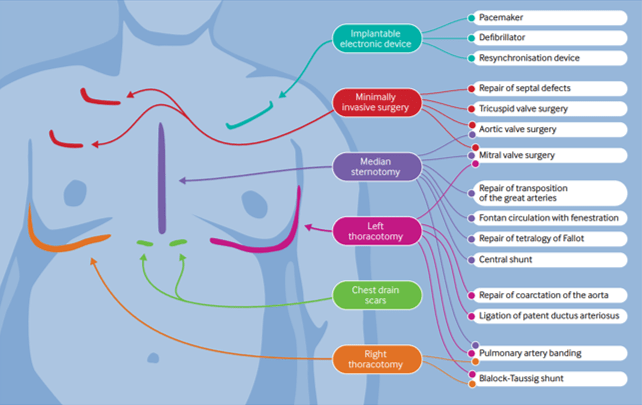
The presence of scars may give you some clues as to the patient's underlying condition and previous surgical repairs. (BMJ 2016; 354: i3905)
A General Approach
- Do your usual ABC assessment.
- Pay particular attention to the respiratory rate - this should be normal.
- Give oxygen if they look unwell.
- They should have a 'normal' blood pressure - any hypotension should be taken as abnormal and investigated.
The Fontan Circulation
This is not a condition in itself, but in fact the resulting circulation after a series of operations that could've been performed due to a number of different underlying conditions:
- Tricuspid Atresia
- Double Inlet Left Ventricle
- Atrio-ventricular Septal Defect – unbalanced
- Pulmonary Atresia
- Hypoplastic Left Heart Syndrome
In essence these patients are born with a single functioning ventricle, that has to be utilised to supply the systemic side of the circulation, whilst the Fontan acts as a passive means of returning blood to the pulmonary circulation.
It was first devised in the early 1970s by Dr Francis Fontan, so the majority of patients with this are in their mid thirties and younger.
Potential reasons for admission to the ED - Fontan circulation
1, Arrythmia
As the patient is entirely dependent on their systemic ventricle to work optimally, any disturbance of the delivery into it is very poorly tolerated. Thus, any arrhythmia is life threatening, even a mild atrial tachycardia.
These patients need to be returned to sinus rhythm as quickly as possible and the recommended method for this is DC cardioversion in expert hands.
Fontan patients have an incredibly fragile circulation and any change in their respiratory physiology can be life threatening, especially if it increases their pulmonary pressures (and thus prevents the passive flow within the Fontan circulation). These patients are not candidates for sedation in the ED and should have an experienced anaesthetist to manage them during the procedure.
Beware if the patient comes in and tells you they are fasted! This means they have been in this situation before and needed DC cardioversion.
2, Haemoptysis
Over time the patient develops venous hypertension within the Fontan connection. This causes the formation of collateral vessels, that may link into the bronchial arterial tree.
If the patient presents in shock treat them as you would any other patient with emergency blood transfusion.
Any haemoptysis, however small, may herald the beginning of a massive bleed. These patients need further investigation, probably a CT chest with contrast. These vessels may then be coiled by interventional radiology.
3, Cyanosis
If the patient has a non fenestrated Fontan they should have normal oxygen saturations. However, if there is a fenestration there will be shunting and therefore a reduction in oxygenation.
For patients this is trade of between being pink or blue, each of which have complications.
Dr Sam Fitzsimmons
Dr Sam Fitzsimmons is a Consultant Cardiologist in Adult Congenital Heart Disease (ACHD) at the University Hospital Southampton, UK. Sam also subspecialises in pulmonary hypertension and maternal cardiology. Working within a tertiary surgical ACHD centre, Sam delivers an ACHD on call service for emergency admissions, inpatient care, routine outpatient follow-up, intra-operative imaging and post-surgical care, as well as specialist clinics in Pulmonary Hypertension and Maternal Cardiology. Sam holds a Honorary Senior Clinical Lecturer post with the University of Southampton as she is passionate about teaching and in particular, she is enthusiastic about helping demystify congenital heart disease for many non-specialist to improve patient care. Sam is well published in peer review journals, cardiology textbooks and specialist guidelines.

No comments yet. Be the first to say something!