
1.3M
Downloads
272
Episodes
A UK based Emergency Medicine podcast for anyone who works in emergency care. The St Emlyn ’s team are all passionate educators and clinicians who strive to bring you the best evidence based education. Our four pillars of learning are evidence-based medicine, clinical excellence, personal development and the philosophical overview of emergency care. We have a strong academic faculty and reputation for high quality education presented through multimedia platforms and articles. St Emlyn’s is a name given to a fictionalised emergency care system. This online clinical space is designed to allow clinical care to be discussed without compromising the safety or confidentiality of patients or clinicians.
Episodes

Saturday Jun 13, 2020
Ep 171 - May 2020 Round Up
Saturday Jun 13, 2020
Saturday Jun 13, 2020
Lots to chat about on the podcast this month, and not just COVID! There's been blog posts about clots, troponin and even telly, as well as the Journal Club series.
Keep a look out for the new St Emlyn's Lesson Plans that we hope will help usher in a new era of medical education in a socially distanced world.
If you would like to donate to the fund in the memory Adel Aziz you can find the link here.
We hope you're finding all of our output useful. Please do subscribe to the website (in the top right hand corner) and rate our podcast on iTunes.
Take care
Iain
Podcast edited by Izzy Carley
PS You can find the Lesson Plans here. Still a work in progress, but as you've read these "shownotes" you deserve to have a sneak preview...

Thursday Jun 04, 2020
Ep 170 - COVID-19 Journal Club #7 (June 2020)
Thursday Jun 04, 2020
Thursday Jun 04, 2020
Welcome to our seventh webinar and journal club reviewing recent research and featuring COVID-19 updates, hosted by the University of Manchester, Manchester Royal Infirmary and Royal College of Emergency Medicine in collaboration with St Emlyn's.
The live event took place on Tuesday 26th May.
Today's panel will be hosted by Rick Body The panel includes Prof Paul Klapper (Professor of Clinical Virology), Dr Charlie Reynard (NIHR Clinical Research Fellow), Dr Anisa Jafar, Prof Pam Vallely (Professor of Medical Virology), Ellie Hothershall (Consultant in Public Health), Prof Simon Carley and special guest Kelly Ann Janssens (Emergency Physician in Ireland) to discuss five papers about COVID-19 infection.
This will be the last weekly journal club, but we will be back with more EBM goodness very soon. Do let us know what you like to be included at stemlyns@gmail.com
References
-
Beigel JH, Tomashek KM, Dodd LE, et al. Remdesivir for the Treatment of Covid-19 — Preliminary Report. N Engl J Med. Published online May 22, 2020. doi:10.1056/nejmoa2007764
-
Mehra MR, Desai SS, Ruschitzka F, Patel AN. Hydroxychloroquine or chloroquine with or without a macrolide for treatment of COVID-19: a multinational registry analysis. The Lancet. Published online May 2020. doi:10.1016/s0140-6736(20)31180-6
-
Gray N, Calleja D, Wimbush A, et al. “No test is better than a bad test”: Impact of diagnostic uncertainty in mass testing on the spread of Covid-19. Published online April 22, 2020. doi:10.1101/2020.04.16.20067884
-
Peyrony O, Marbeuf-Gueye C, Truong V, et al. Accuracy of Emergency Department clinical findings for diagnostic of coronavirus disease-2019. Annals of Emergency Medicine. Published online May 2020. doi:10.1016/j.annemergmed.2020.05.022
-
Ludvigsson JF. Children are unlikely to be the main drivers of the COVID‐19 pandemic – a systematic review. Acta Paediatr. Published online May 19, 2020. doi:10.1111/apa.15371
Friday May 22, 2020
Ep 169 - COVID-19 Journal Club #6 (May 2020)
Friday May 22, 2020
Friday May 22, 2020
Welcome to our sixth COVID-19 Journal Club Podcast.
The panel was hosted by Rick Body and included Prof Paul Klapper (Professor of Clinical Virology), Dr Charlie Reynard (NIHR Clinical Research Fellow), Dr Anisa Jafar, Prof Pam Vallely (Professor of Medical Virology), Prof Simon Carley and special guest Liz Crowe (Advanced Clinician Social Worker and PhD candidate in health staff wellbeing in Brisbane) to discuss four papers about COVID-19 infection. We were especially pleased to welcome Liz this week, which enabled us to focus on the important topics of grief, loss and communication during the COVID-19 pandemic.
References

Wednesday May 13, 2020
Ep 167 - Troponin Update and LoDED Study Review with Rick Body
Wednesday May 13, 2020
Wednesday May 13, 2020
Over the last few years many of us in the UK have started to incorporate high-sensitivity troponin into the assessment of patients presenting with chest pain.
We have seen these samples taken at ever shorter intervals, aiming to discharge low risk patients safely, sooner from the Emergency Department (ED). This has been driven in part by the "Four Hour Emergency Access Target" as well as increased crowding in overwhelmed EDs.
In this podcast, internationally renowned researcher Prof Rick Body discusses the latest in troponin research and the recent LoDED study.
The Shownotes
The various organisations mentioned by Rick can be found here:
The Innovation Agency Webinar Series
The NHS Accelerated Access Collaborative
The CQUIN that will be implemented later this year (page 15 for the Troponin section)
The Draft NICE recommendations
Thursday May 07, 2020
Ep 166 - COVID-19 Journal Club #4 (May 2020)
Thursday May 07, 2020
Thursday May 07, 2020
Welcome to our fourth webinar and journal club reviewing recent research and featuring COVID-19 updates, hosted by the University of Manchester, Manchester Royal Infirmary and Royal College of Emergency Medicine in collaboration with St Emlyn's.
The live event tool place on Tuesday 5th May at 11.30am BST (10.30am GMT).
The panel was again be hosted by Rick Body The panel includes Prof Paul Klapper (Professor of Clinical Virology), Dr Charlie Reynard (NIHR Clinical Research Fellow), Dr Anisa Jafar (Academic Clinical Lecturer), Prof Pam Vallely (Professor of Medical Virology), Prof Simon Carley and special guest Justin Morgenstern to discuss six papers about COVID-19 infection.
There will be another COVID 19 Journal Club next week (Tuesday 12th May at 11am).
References
Podcast edited from a live webinar by Izzy Carley

Sunday May 03, 2020
Ep 165 - April 2020 Round Up
Sunday May 03, 2020
Sunday May 03, 2020
It's been another busy month at St Emlyn's, with the publication of 15 blog posts and five podcasts, but there does seem to be an awful lot to talk about!
Of course there have been multiple posts and podcasts about COVID-19, and you can fiind all of these on our special St Emlyn's page. Highlights have included the three RCEM/St Emlyn's Webinars which we are delighted to host in podcast form.
It's not just been coronavirus though, we have also dipped out toes into exercise and nutrition, graphic design and horticulture!
Parts of the site have also undergone a bit of a redesign with the curriculum pages now easier to navigate to find that post to fioll an e-portfolio hole.
We hope you're finding all of our output useful. Please do subscribe to the website (in the top right hand corner) and rate our podcast on iTunes.
They'll be much more to come in May I am sure.
Take care
Iain
Podcast edited by Izzy Carley
Wednesday Apr 22, 2020
Ep 162 - Beyond the ED: COVID-19 and Critical Care with Dan Horner
Wednesday Apr 22, 2020
Wednesday Apr 22, 2020
In this podcast, Dan and Iain talk about the clinical journey of a COVID-19 patient, beyond the ED, with insights from the critical care unit. There are some concepts here that we don’t have time to do full justice to in the podcast, so there is a comprehensive set of "show notes" and all the references at www.stemlynsblog.org/covid-19-and-critical-care

Sunday Jan 19, 2020
Ep 153 - December 2019 Round Up
Sunday Jan 19, 2020
Sunday Jan 19, 2020
Our regular round up of the best of the blog from December 2019. Published a little late, largely because of Coronavirus issues and general business.
Thursday Nov 14, 2019
Ep 150 - REBOA with Zaf Qasim
Thursday Nov 14, 2019
Thursday Nov 14, 2019
Simon and Zaf talk about the practicalities of REBOA and discuss whether it's ready for prime time in the UK.
Introduction
Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA) is a minimally invasive technique designed to control hemorrhage in patients with life-threatening bleeding and offers a bridge to definitive surgical intervention. Here at St Emlyn’s, we are committed to exploring innovative solutions that enhance patient outcomes in emergency medicine. In this post, we delve into the essentials of REBOA, its clinical application, benefits, and challenges.
Understanding REBOA
REBOA involves the insertion of a balloon catheter into the aorta via the femoral artery. By inflating the balloon, we can occlude the aorta, thus controlling bleeding below the point of occlusion. This procedure is particularly useful in cases of non-compressible torso haemorrhage, where traditional methods of haemorrhage control are inadequate.
Indications and Contraindications
Indications:
- Hemorrhagic shock from pelvic fractures or abdominal bleeding.
- Trauma patients with signs of severe hemorrhage unresponsive to fluid resuscitation.
- As a temporary measure until surgical control of bleeding is achieved.
Contraindications:
- Patients with known aortic pathology (e.g., aortic dissection).
- Significant injury above the diaphragm.
- Prolonged transport times where REBOA may not be beneficial.
The Procedure
Preparation
Before performing REBOA, it is crucial to ensure that the patient is appropriately resuscitated and stabilized as much as possible. This includes securing the airway, ensuring adequate ventilation, and achieving initial hemodynamic stabilization.
Insertion and Inflation
- Vascular Access: Gain access to the common femoral artery using ultrasound guidance to minimize complications.
- Catheter Insertion: Insert the REBOA catheter through a sheath into the femoral artery. Advance the catheter under fluoroscopic or ultrasound guidance to the desired level in the aorta (Zone I: above the celiac artery for abdominal hemorrhage, Zone III: above the bifurcation of the iliac arteries for pelvic hemorrhage).
- Balloon Inflation: Inflate the balloon to occlude the aorta. This temporarily controls bleeding and allows time for definitive surgical repair.
Monitoring and Maintenance
Continuous monitoring of vital signs and catheter position is essential. The occlusion time should be minimized to reduce ischemic complications. Ideally, REBOA should serve as a bridge to definitive surgical intervention within 30-60 minutes.
Benefits and Challenges
Benefits
- Rapid Hemorrhage Control: REBOA can quickly control bleeding, buying crucial time for surgical intervention.
- Less Invasive: Compared to traditional open thoracotomy with aortic cross-clamping, REBOA is less invasive, reducing associated morbidity.
- Improved Survival Rates: Emerging evidence suggests that REBOA can improve survival rates in appropriately selected trauma patients.
Challenges
- Technical Expertise: REBOA requires specific training and expertise. Improper technique can lead to significant complications.
- Ischemic Complications: Prolonged aortic occlusion can lead to ischemia of distal organs and tissues, necessitating careful monitoring and timely deflation.
- Resource Intensive: REBOA demands resources such as fluoroscopy, ultrasound, and trained personnel, which may not be available in all settings.
Conclusion
REBOA represents a promising advancement in trauma care, offering a vital tool in the management of life-threatening haemorrhage, but it's utility in the Emergency Department is uncertain.
Further reading

Thursday May 30, 2019
Ep 137 - Beyond ATLS with Alan Grayson at #stemlynsLIVE
Thursday May 30, 2019
Thursday May 30, 2019
Alan Grayson takes us through his thoughts on ATLS. Is it really as terrible the #FOAMed world makes out?

Sunday May 19, 2019
Ep 136 - Wellbeing for the broken with Liz Crowe
Sunday May 19, 2019
Sunday May 19, 2019
Navigating a Mental Health Crisis in Healthcare: A Guide to Recovery
Healthcare professionals, particularly those working in critical care and emergency medicine, often face intense situations that test their emotional and mental resilience. While most of the time, we manage to cope with the challenges, there are rare moments that catch us completely off guard, leaving us feeling utterly broken. This guide explores what to do when work breaks you—a situation that is seldom discussed but is profoundly important.
Understanding the Crisis Point
It's crucial to distinguish between the routine stressors of healthcare work and a true mental health crisis. The latter is not just a rough day or a series of challenging weeks. Instead, it's a once-in-a-career event that completely shakes your confidence and leaves you questioning your ability to continue in your role. These moments can be triggered by traumatic patient cases, critical errors, or cumulative stress that finally overwhelms you.
When such a crisis occurs, it’s important to recognize that what you're experiencing goes beyond normal stress—it’s a mental health crisis. Symptoms may include tremors, uncontrollable crying, sleeplessness, and a sense of detachment. These are signs that your mental health is under severe strain, and they should be taken seriously.
Preparing for a Crisis Before It Happens
One of the most valuable steps you can take is to prepare for the possibility of a mental health crisis before it happens. Just as we plan for emergencies in our professional roles, we should also have a plan in place for our mental well-being.
1. Build a Support Network: Identify a few trusted individuals—whether colleagues, friends, or family—who can be your go-to support in times of crisis. Share with them the kinds of situations that might overwhelm you and how they can help if the time comes.
2. Establish a Routine: Develop a daily routine that includes exercise, healthy eating, and regular sleep. Routine can serve as a stabilizing force during a crisis, providing a sense of normalcy when everything else feels chaotic.
3. Seek Professional Help: It’s wise to establish a relationship with a therapist or counsellor before a crisis hits so you have someone to turn to when you need it. If therapy isn’t an option, know how to access support through your GP or other services.
4. Practice Self-Care: Identify activities that help you relax and de-stress. Whether it’s meditation, reading, or spending time with loved ones, incorporate these into your routine. These activities can become particularly crucial during a crisis.
What to Do During a Crisis
When you find yourself in the midst of a mental health crisis, your judgment may be impaired, making it difficult to make decisions or know what to do next. Here’s how to navigate those critical moments:
1. Reach Out for Support: Even though your instinct may be to withdraw, it’s essential to reach out to someone in your support network. Connection is key to navigating a crisis. Tell them what’s happened and how you’re feeling, even if it feels incredibly difficult to do so.
2. Stick to Your Routine: Maintain your daily routine as much as possible, even if it feels challenging. Simple actions like getting up at the same time, eating regular meals, and exercising can help you regain a sense of control.
3. Avoid Self-Medication: The temptation to numb your feelings with alcohol, drugs, or other substances can be strong during a crisis. However, these can exacerbate the situation. If you feel the need for medication, consult with a healthcare professional instead of self-medicating.
4. Seek Professional Help: If you’re struggling to cope, don’t hesitate to seek professional assistance. Talking to a professional, whether through your GP, a therapist, or a crisis hotline, can provide the validation and support you need.
The Path to Recovery
Once the immediate crisis has passed, the journey to recovery begins. This process is often slow and requires patience, self-compassion, and continued support.
1. Allow Yourself Time: Recovery from a work-related mental health crisis takes time, often longer than expected. Be patient with yourself and understand that healing is a gradual process that may take months or even years.
2. Maintain Your Routine: Continue the routine that helped you during the crisis. Regular exercise, healthy eating, and sufficient sleep are the foundations of good mental health and will support your recovery.
3. Reconnect with Your Purpose: Reflect on why you chose your profession and what you love about your job. Reconnecting with these motivations can help you find meaning and purpose again, even after a traumatic experience.
4. Set Small Goals: During your recovery, set small, achievable goals rather than overwhelming yourself with big plans. Celebrate small victories, whether it’s getting through a day at work, completing a project, or simply feeling a bit better.
5. Practice Self-Compassion: Treat yourself with the same compassion you would offer a friend or colleague going through a similar situation. Acknowledge your progress, and don’t be too hard on yourself if recovery takes longer than expected.
Dealing with Shame and Guilt
One of the most challenging aspects of recovery is dealing with feelings of shame and guilt, which can be powerful and difficult to overcome.
1. Acknowledge Your Feelings: It’s normal to feel shame and guilt after a traumatic event, but also understand that these feelings are often irrational and not based on reality.
2. Challenge Negative Thoughts: When feelings of shame or guilt arise, challenge them by asking yourself if they are truly justified. Often, these feelings are rooted in distorted thinking patterns that can be corrected.
3. Talk About It: Sharing your feelings with someone you trust can help alleviate the burden of shame and guilt. Expressing these emotions can reduce their power over you and facilitate healing.
4. Focus on the Positive: Remind yourself of all the good you’ve done in your career. Think about the lives you’ve touched and the positive impact you’ve had. Your career is more than just one event; it’s a series of contributions that define your professional journey.
Moving Forward
At St. Emlyn’s, we believe that your narrative as a healthcare professional is not defined by a single event. You are more than the challenges you’ve faced, and you have the strength to overcome even the most difficult moments. Remember that you are part of a community that understands what you’re going through and is here to support you.
1. Stay Connected: Don’t let the crisis isolate you. Stay connected with your colleagues, friends, and family, who can provide support, perspective, and encouragement as you move forward.
2. Keep Learning: Use your experience as an opportunity for growth. Reflect on what you can learn from the crisis and how it can make you a better healthcare professional.
3. Be Compassionate: Always remember to be compassionate towards yourself. Healing from a work-related mental health crisis is not easy, but with time, support, and self-care, you can emerge stronger and more resilient.
Conclusion
If you’ve experienced or are currently going through a mental health crisis due to work, know that you are not alone. The feelings of being broken, the shame, the guilt, and the fear are all part of the process—but they do not define you. By preparing in advance, seeking support, and practising self-compassion, you can navigate even the darkest moments.
At St. Emlyn’s, we’re here to remind you that your worth is not measured by your worst days. Your career is a journey, and while it may have its challenges, it is also filled with moments of profound impact, healing, and growth. Take the time to care for yourself, to heal, and to reconnect with your purpose. You are important, and your work is valued.

Wednesday Apr 10, 2019
Ep 132 - Aortic Emergencies with George Wills at #stemlynsLIVE
Wednesday Apr 10, 2019
Wednesday Apr 10, 2019
Back in late 2018 we gathered in Manchester for the inaugural #stemlynsLIVE conference. Our friend Dr George Wills gave a great talk on Aortic Emergencies.
All emergency physicians know that it's all to easy to miss an aortic catastrophe. Listen to George's wisdom on common pitfalls and top tips to make you a better emergency clinician.
vb
S
Also check out these excellent #FOAMed resources.
- Subscribe to the blog (look top right for the link)
- Subscribe to our PODCAST on iTunes
- Follow us on twitter @stemlyns
- PLEASE Like us on Facebook
- Find out more about the St.Emlyn’s team

Friday Jan 11, 2019
Ep 127 - The Journey that Matters with Clare Richmond at #stemlynsLIVE
Friday Jan 11, 2019
Friday Jan 11, 2019
This podcast and presentation was recorded at the St Emlyn's LIVE conference in Manchester 2018. In this presentation Clare takes us through the rationale, principles, training and practice that we need in order to continually develop as prehospital and resuscitation practitioners.
You can read more from the event at http://www.stemlynsblog.org
This is a great presentation for anyone interested in continually developing their own and their colleagues practice, delivered by someone who really knows what they are talking about and who works for one of the best developed resuscitation services in the world.
Clare is an Emergency Physician and specialist in Pre-Hospital Care and Retrieval medicine based in Sydney, with Royal Prince Alfred Hospital and Sydney HEMS. She has completed a fellowship in simulation based education, and enjoys training with “real” people - patients, bystanders and the other clinicians we come across as we treat our patients every day. She is a lecturer with the University of Sydney, and is involved in education for the NSW Institute for Trauma Injury Management. When Clare is not working on helicopters or training teams, she is studying yoga or hanging out with her puppy, Archie.

Sunday Dec 23, 2018
Ep 125 - November 2018 Round Up
Sunday Dec 23, 2018
Sunday Dec 23, 2018
St Emlyn's November 2018 Review: Key Highlights and Insights
Hello and welcome to the St Emlyn's Podcast and blog. I'm Simon Carley, and I'll be guiding you through the exciting topics and developments we've covered on the blog in November 2018. From leadership insights to groundbreaking medical research, this month has been incredibly informative. Let's dive into the highlights!
Leadership Insights from the FIX Conference
We begin our review in New York, where Natalie May attended the FIX (FeminEM) Conference. In her second post about this event, Natalie explores profound themes, particularly around leadership and motivation in the medical field.
Key Takeaways on Leadership and Motivation
Jennifer Walthall's talk emphasized the importance of acting within the system to drive change. When joining an organization that may not align with your values, you can either work within the system to improve it or fight from the outside. Walthall advocates for influencing change from within, suggesting that once embedded, you can effectively drive improvements.
Lara Goldstein's session on leadership identified four critical attributes of a good leader:
- Listening: Truly understanding your team.
- Recognizing the Impact of Small Actions: Little things add up.
- Conflict Management: Not everyone will like you, and that's okay.
- Gratitude, Kindness, and Decency: Core values that should guide every leader.
Natalie's detailed reflections on the FIX Conference are a must-read for those interested in these themes. Attending FIX in 2019 should be on your list if possible!
POLAR Trial: New Insights into Hypothermia Post-Brain Injury
Dan Horner analyzed the POLAR trial in one of our journal club posts. The POLAR trial is a significant randomized control trial investigating the effects of hypothermia in the early stages after a brain injury. This study follows the Eurotherm trial, which explored hypothermia's role in patients with severe brain injuries in the ICU.
What the POLAR Trial Reveals
The POLAR trial involved 511 patients with severe brain injuries, randomized to either hypothermia (cooling to 33-35°C) or maintaining normothermia for 72 hours. Despite strong pathophysiological evidence supporting hypothermia, the trial found no significant difference in outcomes after six months. Initial results suggest that routine hypothermia for early-stage brain injury might not be beneficial, but long-term data follow-up is crucial. This trial, published in JAMA, is essential reading for anyone involved in emergency medicine or critical care.
The Case for Whole Blood Transfusion in Trauma: Insights from Zaf Qasim
Zaf Qasim, a former Manchester trainee now making waves in the US, contributed an enlightening post on the use of whole blood in trauma resuscitation. This approach, which makes intuitive sense—replacing lost whole blood with whole blood—contrasts with the UK practice of separating blood into components for transfusion.
Advantages of Whole Blood Transfusion
Zaf argues that whole blood could simplify and improve trauma care, reducing the time and complexity of reconstituting blood components in the body. Although not yet standard in the UK, this method is gaining traction in places like London HEMS and various European centers. As data continues to emerge, this could revolutionize trauma care, harkening back to practices from the Second World War and Vietnam.
Challenging the Use of "Sexy" in Clinical Medicine
Natalie May returns with a provocative post challenging the use of the term "sexy" in clinical medicine, especially in resuscitation-related specialties. Often used to describe procedures or equipment, this term can inadvertently perpetuate gender biases and undermine professionalism.
Redefining Professional Language
Natalie, supported by her husband Oli May's humorous yet insightful critique, urges us to reconsider such language. The term "sexy" in a medical context is not a compliment and can contribute to a culture that sexualizes women in the workplace. This reflection is especially relevant for departments striving to maintain professionalism and inclusivity.
Understanding Cognitive Load Theory with Nick Smith
In the realm of medical education, Nick Smith's debut blog post introduces us to cognitive load theory. As a clinical educator in Manchester, Nick explores how intrinsic, extrinsic, and germane cognitive loads affect learning and teaching.
Applying Cognitive Load Theory in Medical Education
Nick's post is a valuable resource for educators aiming to optimize their teaching strategies. By understanding and managing cognitive load, we can create more effective and supportive learning environments for our trainees. This post is part of a broader series on educational theories that are crucial for medical educators.
Elective Experience in South Africa: Lessons from Claire Bromley
Medical student Claire Bromley shares her transformative elective experience at Mitchell's Plain with the BAD EM team. Working with leaders like Katya Evans and Craig Wylie, Claire's reflections offer deep insights into the challenges and rewards of emergency medicine in South Africa.
Bridging UK Training with South African Realities
Claire highlights the stark differences between UK and South African healthcare systems, particularly the intense workload and resource constraints in the public sector. Her experience underscores the importance of preparation, respect, and adaptability for anyone considering working in a different health economy.
Promoting Diversity in the Emergency Department
Natalie May's final post for November reflects on promoting diversity and inclusivity in the emergency department. She emphasizes that the ED is unique in its diversity, seeing patients from all walks of life.
Embracing and Understanding Diversity
Natalie advocates for a broader understanding of diversity beyond ethnicity, including gender, disability, and sexual orientation. Her insights are essential for ED professionals committed to providing equitable care and fostering an inclusive environment.
Learning in the Social Age: Embracing Medutainment
I had the pleasure of discussing "Learning in the Social Age" at the Emerge 10 conference in Scotland. This presentation, supported by a blog post, explores how the internet and social media are transforming medical education.
The Impact of Medutainment
We are now competing on a global scale as educators, with learners accessing information from various sources worldwide. This shift necessitates embracing new methods of engagement, ensuring our teaching remains relevant and impactful.
Beyond ALS: Innovations in Cardiac Arrest Management
We wrapped up November with a highlight from St Emlyn's Live, featuring Salim Rezaie from the RebelEM blog and podcast. Salim's presentation on "Beyond ALS" challenges us to rethink cardiac arrest management, focusing on advanced techniques and evidence-based practices.
Advancing Cardiac Arrest Protocols
Salim's talk covers crucial aspects such as minimizing shock pauses, effective adrenaline administration, and optimizing IV/IO access. For anyone serious about improving their ALS skills, this blog, podcast, and accompanying videos are indispensable resources.
Looking Ahead
November was a whirlwind of activity and learning at St Emlyn's, and we have plenty more in store for December. As we approach the holiday season, we hope you find time to explore these posts and integrate their lessons into your practice. Thank you for being part of the St Emlyn's community, and we look forward to continuing this journey of learning and improvement together.
Wednesday Nov 28, 2018
Ep 122 - Beyond ALS with Salim Rezaie at #stemlynsLIVE
Wednesday Nov 28, 2018
Wednesday Nov 28, 2018
Salim Rezaie from the REBEL EM podcast takes us through the optimal management of cardiac arrest and also explores some of the controversies and difficulties that make the difference to our patients.
You can read a lot more about the background to this talk, see the evidence and watch the video on the St Emlyn's site. Just follow this link. https://www.stemlynsblog.org/beyond-acls-salim-rezaie-at-stemlynslive/

Sunday Oct 28, 2018
Ep 120 - The pursuit of excellence with Nat May at #stemlynsLIVE
Sunday Oct 28, 2018
Sunday Oct 28, 2018
This presentation was given at the inaugural #stemlynsLIVE conference on the 8th of October 2018 in Manchester. You can read more about the presentation and the conference here. https://www.stemlynsblog.org/in-pursuit-of-excellence/

Tuesday Apr 24, 2018
Ep 108 - February 2018 Round Up
Tuesday Apr 24, 2018
Tuesday Apr 24, 2018
Monthly Update from St. Emlyn’s: Insights into Emergency Medicine
Welcome to the St. Emlyn’s podcast blog! I’m Ian Beardsell, and alongside Simon Cully, we're here to bring you our monthly update. This post will delve into February's content, upcoming events, and the latest discussions in emergency medicine.
Winter Challenges and Patient Updates
Winter has been relentless this year, and we're still feeling its impact. The influx of patients hasn't slowed down, and our departments are buzzing with activity. Up in Manchester, we continue to see a high volume of patients, while down south, the weather has been kinder, though no less busy. As a Yorkshireman, I can empathize with the challenges faced in the North. Hang in there, and let's get through these cold evenings together!
Upcoming Events: St. Emlyn’s Live and Teaching Course
Before diving into February's posts, let's talk about the exciting events we have lined up. This October, we're hosting the St. Emlyn’s Live conference and the Teaching Course in Manchester.
St. Emlyn’s Live Conference
The St. Emlyn’s Live conference is a one-day event focused on our philosophy's four pillars: clinical work, evidence-based medicine, wellbeing, and the philosophy of emergency medicine. With international speakers, this event promises to be an enriching experience for all attendees. Spaces are limited, so make sure to book your spot early via our website.
Teaching Course in Manchester
Following the conference, we have a three-day Teaching Course designed to develop you as an expert teacher in emergency medicine. This comprehensive course covers all aspects of teaching and is an excellent opportunity to enhance your skills. All bookings can be made through the St. Emlyn’s website.
Insights from February’s Blog Posts
February was a month rich with valuable insights and studies. Let's delve into some of the highlights:
Intranasal Ketamine and Fentanyl for Children
One of the standout studies we reviewed in February focused on the use of intranasal ketamine and fentanyl for managing pain in children. Pain management in pediatric patients is always challenging, especially when IV access is difficult. Traditionally, we've used intranasal diamorphine, but there's been a shift towards using intranasal ketamine and fentanyl, particularly in the US.
Study Overview
This randomized controlled trial compared 1 mg/kg of intranasal ketamine against 1.5 mcg/kg of intranasal fentanyl in children aged 4 to 17 with suspected isolated extremity fractures. The primary outcome was pain reduction, and both drugs performed similarly in this regard.
Side Effect Profiles
The key takeaway was the difference in side effect profiles. Ketamine is known to cause dysphoria, vomiting, and dizziness, while fentanyl has fewer unpleasant side effects. Therefore, fentanyl emerged as the preferred choice not because of superior pain relief but due to its more favourable side effect profile.
Practical Implications
The study underscores the importance of having a streamlined protocol for intranasal medications in emergency departments. While some departments might still use syringes, investing in mucosal atomizer devices can simplify administration and improve patient care.
Engaging Medical Students in Emergency Medicine
We had a guest blog from Claire Bromley, a medical student working with us in Manchester. Claire shared her experiences and insights into why she chose emergency medicine as a career, despite the occasional negativity she faced from other specialties.
Building a Career in Emergency Medicine
Claire's blog is an inspiring read for medical students considering a career in emergency medicine. She highlights the importance of engaging students in the department and ensuring they see the undifferentiated, unwell patients that characterize our specialty. Her experiences as a SMACC volunteer and her early involvement in FOAMed (Free Open Access Medical Education) are testaments to the value of early engagement and online education.
The Role of Educators
One of the significant challenges we face is balancing the educational needs of students with the operational demands of the department. However, investing time in student education is crucial. These students are our future colleagues, and their early exposure to emergency medicine can shape their career choices and prepare them for the challenges ahead.
Aromatherapy with Isopropyl Alcohol for Nausea
A fascinating study we reviewed involved the use of isopropyl alcohol for nausea relief. The concept of sniffing alcohol swabs to alleviate nausea isn't new, but this study provided robust evidence supporting its effectiveness.
Study Design and Results
The randomized controlled trial compared the effects of isopropyl alcohol sniffing to oral ondansetron in adult patients presenting with nausea in the emergency department. The results were surprising: patients who sniffed isopropyl alcohol swabs reported greater relief from nausea than those who took ondansetron.
Implementation Challenges
While the study's findings are promising, implementing this practice consistently in emergency departments can be challenging. Ensuring that alcohol swabs are readily available and that staff are trained to use them effectively is key. Additionally, clarifying whether a Patient Group Directive (PGD) is required for this intervention could streamline its adoption.
Reflections on Historical Practices
One of the lighter yet insightful pieces this month was a video from the 1970s showcasing a casualty department in Liverpool. Watching historical medical practices can be both amusing and educational, offering a perspective on how far we've come and what future generations might think of our current practices.
Educational Value
While humorous at times, the video also highlights the core principles of emergency medicine that remain unchanged. It reminds us of the importance of continuous learning and adaptation in our field.
Looking Ahead: SMACC 2019 and Beyond
As we look forward to the year ahead, we’re excited about the upcoming SMACC conference in Australia in 2019. Planning for study leave and participation in such international conferences is essential for continuous professional development. These events provide unparalleled opportunities for learning, networking, and sharing best practices.
Conclusion
February has been a month filled with valuable insights, studies, and preparations for future events. The emphasis on pain management in children, engaging medical students, and innovative approaches to nausea relief reflects our ongoing commitment to improving patient care and education in emergency medicine.

Monday Apr 02, 2018
Ep 107 - January 2018 Round Up
Monday Apr 02, 2018
Monday Apr 02, 2018
Surviving a Relentless Winter: Reflections and Insights from St. Emlyn's
Welcome Back to the St. Emlyn's Podcast
Welcome to the St. Emlyn's podcast. I'm Iain Beardsell, and I'm Simon Carley. We are delighted to be back with you after what can only be described as a rather tricky winter. The winter season has always been challenging for emergency departments across the UK, but this year felt especially relentless. In this blog post, we will reflect on the past few months, share key insights, and look forward to exciting events on the horizon, including the St. Emlyn's Live conference.
The Winter Struggle: A Nationwide Challenge
Down south in our emergency department, we have faced significant challenges. Iain shared his experiences: "We have been having a heck of a time. It has been a real struggle. I'm utterly exhausted, and it has only been in the last couple of weeks that it felt like we could breathe again." The situation has been similarly difficult up north. Simon echoed these sentiments: "It's been a bit grim up north, to be honest. This winter felt different, harder. The emergency departments in the UK have always had problems over winter, but it has felt more relentless this year."
Unprecedented Pressure and Relentless Demand
We didn't have much of a summer to recuperate, and the winter was relentless day in and day out. Our department saw unprecedented pressure, with patient numbers pushing us to our limits. Interesting statistics from our department showed consecutive days of being over capacity, creating concerns about patient care and safety. Despite the exhaustion, we managed to maintain a high standard of care, with complaints remaining at normal levels and even receiving more compliments than usual.
Coping Strategies and Positive Outcomes
Maintaining patient care while looking after ourselves has been a challenge. We have implemented various strategies to keep on track, from educational events to incredible clinical work. Reflecting on our achievements, Simon highlighted the importance of continuing education and maintaining healthcare standards even under pressure. "We have done some amazing things over the winter, and it is something we can be really proud of," he said.
Understanding Public Perception and Political Activity
The public's understanding of the pressures in the healthcare system has increased, although tolerance for the challenges faced remains limited. Political activity over the winter saw clinical leads writing to the Prime Minister, and emergency medicine frequently made the front pages of newspapers. However, recent events, such as the nerve agent attack in Salisbury, have shifted the focus away from A&E crowded corridors, providing some relief.
Looking Forward to St. Emlyn's Live
We have many exciting events coming up this year, including the highly anticipated St. Emlyn's Live conference. Scheduled for Tuesday, the 9th of October in Manchester, this one-day conference will bring us out from behind our microphones and keyboards to present live. The event promises to be hugely cost-effective, with an incredible lineup of speakers from around the world, including Claire Richmond from Sydney Hems, Natalie May, Salim Rezy from the US, and Kat Evans from South Africa.
Interactive Learning and Cost-Effective Education
We have designed St. Emlyn's Live to be an interactive conference, reflecting everything we aim for in our podcasts and blogs. The conference is priced at £150 for consultants, with discounts available for trainees, registrars, doctors in training, allied health professionals, nurses, and medical students. Given the limited venue size, we expect tickets to sell out quickly, so we encourage early booking.
Post-Conference Teaching Course
For those looking for more in-depth learning, we are hosting a teaching course on the 10th and 11th of October, directly after the conference. This course focuses on practical education techniques, helping clinician educators improve their teaching skills. It has been highly acclaimed by previous participants, offering a transformative learning experience.
Reflecting on Clinical Medicine and Evidence-Based Practice
At St. Emlyn's, we value reflection and evidence-based practice. In January, we covered several important topics on our blog, including devastating brain injuries, dizzy patients, and the adrenal trial. Let's delve into these discussions and see what we can learn.
Devastating Brain Injuries: Updated Guidance
One of the critical topics we discussed was devastating brain injuries. Historically, decisions about the prognosis of patients with severe traumatic injuries or subarachnoid bleeds were often made too quickly, based on initial CT scans. However, recent guidance suggests that we should not make precipitous decisions about patient outcomes solely based on early imaging.
In summary, it's essential to give these patients at least 24 to 72 hours before making a prognosis. This allows time for clinical outcomes to become more apparent. In our hospital, we transfer these patients to neuro-intensive care and have a proactive organ donation program, ensuring patients and their families receive the care they deserve.
Differentiating Dizziness: Central vs. Peripheral Causes
Another challenging area in emergency medicine is dealing with patients presenting with dizziness or vertigo. Differentiating between central causes, such as posterior circulation strokes, and peripheral causes can be difficult but crucial. We highlighted the importance of understanding the difference and utilizing tests like the HINTS exam to aid diagnosis.
As emergency physicians, we must continue to educate ourselves on these diagnostic tools. Utilizing resources like the St. Emlyn's blog, YouTube, and FOAMed can help us stay updated and improve patient care. It's essential to be comfortable revisiting and revising our knowledge to ensure accurate diagnoses and appropriate treatment plans.
The Importance of Reflection in Medical Practice
Reflection is a powerful tool for lifelong learning and self-improvement. Despite recent controversies, such as the case involving a junior doctor in Leicester, we must not abandon reflection. It helps us increase self-awareness, think critically about our practices, and improve our clinical skills.
Natalie May's blog post on reflection emphasizes that it's not just about ticking boxes but about purposeful and structured thinking. Her insights from Sydney Hems highlight the importance of integrating reflection into our daily practice to enhance our growth as clinicians.
The Adrenal Trial: Steroids in Septic Shock
The adrenal trial, reviewed by Dan Horner, examined the use of steroids in septic shock. Published in the New England Journal of Medicine, this trial aimed to determine whether steroids improve outcomes in these patients. The results showed no significant difference in mortality, although some secondary outcomes, such as vasopressor use and ICU days, showed variations.
The trial highlights the complexity of medical treatment and the need for continuous learning and evaluation. It reminds us that while some treatments may show promise, their benefits might not always be clear-cut. This underscores the importance of evidence-based practice and staying informed about the latest research.
Embracing Continuous Learning and Collaboration
Emergency medicine is a dynamic and ever-evolving field. At St. Emlyn's, we are committed to continuous learning, sharing knowledge, and improving patient care. The challenges of winter have tested our resilience, but they have also shown the importance of collaboration, education, and maintaining high standards of care.
We encourage our readers and listeners to stay engaged with our content, participate in upcoming events, and continue striving for excellence in their practice. The St. Emlyn's Live conference and the teaching course are excellent opportunities for professional development and networking with peers from around the world.
Conclusion: Looking Ahead with Optimism
As we move forward into the spring and summer, let's take a moment to reflect on the lessons learned and the progress made. The past winter was tough, but it also demonstrated our ability to adapt, innovate, and support one another. With exciting events like St. Emlyn's Live on the horizon, we have much to look forward to.
Thank you for being part of the St. Emlyn's community. Stay connected, stay curious, and let's continue to learn and grow together. Here's to a bright and hopeful future in emergency medicine.

Wednesday Jan 24, 2018
Wednesday Jan 24, 2018
Understanding Devastating Brain Injury: Key Insights and Guidelines
In a recent episode of the St Emlyn's podcast, Simon Carley hosted experts Dan Harvey and Mark Wilson to discuss the intricacies of managing devastating brain injury (DBI). The conversation covered new guidelines, the challenges in prognostication, ethical considerations, and practical approaches in clinical settings. This blog post provides a comprehensive summary of their insights, focusing on the importance of standardized care, ethical decision-making, and the role of family involvement.
Defining Devastating Brain Injury
Devastating brain injury encompasses severe brain damage that often leads to significant long-term impairment or death. These injuries can result from various causes, including trauma, subarachnoid hemorrhage, hypoxic brain injury, and intracerebral hematomas. The term "devastating" highlights the severity of these injuries, but as discussed, the perception of devastation can vary, complicating management and prognostication.
The Challenge of Prognostication
One of the core issues in managing DBI is the variability in clinical practice across different healthcare settings. This inconsistency can lead to different outcomes depending on where the patient is treated. Dan Harvey emphasized that the new guidelines aim to standardize care, providing a consistent approach regardless of location. The guidelines recommend an observation period of up to 72 hours to gather comprehensive clinical data, crucial for making informed decisions.
Mark Wilson highlighted the difficulty in early prognostication, noting that initial presentations can be misleading. Factors such as intoxication, medication effects, or pre-existing conditions can obscure the true extent of brain injury. The term "perceived devastating brain injury" underscores the subjective nature of these assessments, stressing that what appears catastrophic on imaging may not always align with clinical outcomes.
The Role of Radiology and Clinical Assessment
Radiological findings, while essential, must be interpreted alongside clinical assessments. A severe CT scan may not always correlate with poor clinical outcomes, and vice versa. The discussion stressed the importance of not rushing to judgment based solely on initial imaging or clinical presentation. Recent studies, including those by Hanni Marcus and Mark Wilson, have shown that some patients with poor prognostic indicators can recover better than expected, particularly those with extra-axial hematomas.
Ethical Considerations and Family Involvement
Ethical considerations are paramount in managing DBI. The definition of a "good recovery" can vary widely among patients and families. For example, elderly patients with significant impairments may still value life, even with extensive care needs. The guidelines emphasize the importance of involving families in discussions about prognosis and treatment, ensuring decisions align with the patient's values and preferences.
Understanding the patient's and family's perspectives is crucial in determining the appropriate course of action. This holistic approach ensures that care decisions are not only medically sound but also ethically and personally appropriate. The discussion also highlighted the need for clear communication, helping families navigate complex and emotionally charged situations.
The Importance of Time and Observation
The guidelines advocate for a period of observation to avoid hasty decisions based on incomplete information. This period, typically up to 72 hours, allows for the identification and management of reversible factors, collection of comprehensive medical history, and better communication with the family. The aim is to reduce the risk of prematurely withdrawing life-sustaining treatment.
Practical Decision-Making
Determining the level of care for DBI patients involves deciding whether to transfer them to neurocritical care units or manage them in general ICUs. While specialized care offers advanced interventions like intracranial pressure (ICP) monitoring, evidence does not conclusively show that these measures always improve outcomes. The discussion acknowledged the limitations of resources and the importance of considering logistical factors, such as proximity to the patient's family.
The guidelines encourage clinicians to make informed decisions based on available evidence and specific case circumstances. They stress that not all DBI patients require transfer to specialized centers, especially when prognosis remains uncertain. The focus should be on providing essential life-saving therapies and monitoring the patient's condition.
Transitioning to Palliative Care
When recovery is deemed unlikely, transitioning to palliative care becomes a compassionate and appropriate choice. The guidelines stress the importance of clear communication with the family, ensuring they understand the prognosis and rationale behind limiting or withdrawing aggressive treatment. Palliative care focuses on symptom management, comfort, and supporting the patient and family, addressing not only physical but also emotional and psychological needs.
Organ Donation Considerations
Organ donation is an important consideration for DBI patients when the prognosis is poor. The guidelines recommend discussing this option with the family as part of end-of-life care planning. These discussions should be handled sensitively, providing clear information and respecting the family's wishes. Organ donation can provide hope and purpose in the face of tragedy, potentially saving other lives.
Conclusion and Key Takeaways
The St Emlyn's podcast episode on devastating brain injury provides crucial insights into the complexities of managing this challenging condition. The newly published guidelines offer a structured approach, emphasizing comprehensive assessment, ethical considerations, and family involvement.
Key Takeaways:
-
Standardize Practice: Reduce variability in DBI management by adhering to standardized guidelines, ensuring consistent and high-quality care.
-
Comprehensive Assessment: Utilize both clinical and radiological assessments to inform prognosis. Avoid premature conclusions based on incomplete data.
-
Ethical and Family Considerations: Engage with families to align treatment decisions with the patient's values and wishes. Provide clear, compassionate communication throughout the process.
-
Observation Period: Allow an appropriate observation period to clarify the patient's condition and potential for recovery.
-
Palliative Care: Transition to palliative care when necessary, prioritizing patient comfort and dignity.
-
Organ Donation: Discuss organ donation as part of end-of-life planning, handling these conversations with care and respect.
By following these guidelines, healthcare professionals can navigate the complexities of managing DBI with greater confidence and compassion, ultimately improving patient outcomes and supporting families through challenging times. For more detailed information and resources, visit the St Emlyn's blog and stay updated with the latest in emergency and critical care.
Wednesday Aug 02, 2017
About us
Wednesday Aug 02, 2017
Wednesday Aug 02, 2017
St.Emlyn's is a virtual hospital based in Virchester.
In reality we are a team of Emergency Physicians, friends and colleagues interested in medical education, emergency medicine and critical care. We blog because education matters. Our numbers are growing every day... please feel free to contact us.
Senior Editors
 Professor Simon Carley FOAM(Ed) Professor Simon Carley FOAM(Ed)Professor of Emergency Medicine, Manchester Metropolitan University; Consultant in Emergency Medicine. Co- founder of BestBets, StEmlyns, MSc in EM and other stuff. Research interests in diagnostics, MedEd, Major incidents & Evidence based Emergency Medicine. *Read Posts* | |||
 Professor Rick Body MB ChB, MRCSEd(A&E), FCEM, PhD Professor Rick Body MB ChB, MRCSEd(A&E), FCEM, PhDConsultant in Emergency Medicine at Manchester Royal Infirmary and Honorary Lecturer in Cardiovascular Medicine at the University of Manchester. Major research interests are in the early diagnosis of acute coronary syndromes and humane approaches to improving patient well-being in the ED. Methodological expertise in clinical decision rules, diagnostic studies and cohort studies. - Research - Blog - *Read Posts* |
Editorial Board
 Dr Natalie May MBChB, MPHe, MSc, MCEM, FCEM Dr Natalie May MBChB, MPHe, MSc, MCEM, FCEMConsultant Emergency Physician with speciality training in Paediatric Emergency Medicine, currently working in Prehospital and Retrieval Medicine at Sydney HEMS. Numerous interests in medical education, leadership and emergency paediatrics. #FOAMaoke queen, obsessed with running. *Read Posts* | |||
 Dr Iain Beardsell FOAM(Ed) Dr Iain Beardsell FOAM(Ed)Consultant in Emergency Medicine and Clinical Lead, University Hospitals Southampton and HIOWW HEMS doctor. A passionate advocate for EM with a cup that is (almost) always half full. *Read Posts* |
| ||
 Dr Alan Grayson Dr Alan GraysonGrumpy, balding Yorkshireman, who despite practising medicine on the good folk of Manchester and its environs, still lives in god's own county, after a brief sabbatical learning medicine in Edinburgh and then training in EM in Newcastle and NW England. Has an unhealthy interest in bikes, pies, cricket and Huddersfield Town FC. *Read Posts* | |||
 Dr Richard Carden BSc, MSc, MBChB, MRCEM, RAMC(V) Dr Richard Carden BSc, MSc, MBChB, MRCEM, RAMC(V)Emergency Medicine trainee. Captain in the Royal Army Medical Corps. (Reserves). Former MSc Trauma Sciences (Military and Austere) student, impending Centre for Trauma Sciences PhD student, current Diploma in Medical Care of Catastrophes student. Interested in trauma, toxicology, psychology, physiology and critical care. Trainee rep on the St.Emlyn's team. *Read Posts* | |||
 Dr Janos Peter Baombe MD FRCEM FEBEEM PgCert MSc Dr Janos Peter Baombe MD FRCEM FEBEEM PgCert MScEmergency medicine consultant, Manchester Royal Infirmary. Fellow of the Royal College of Emergency Medicine. Passionate about european EM networks, infectious disease outbreaks and ED preparedness, ultrasonography. World traveller and keen sportsman. *Read Posts* | |||
 Liz Crowe BSW PhD Candidate Liz Crowe BSW PhD CandidateAdvanced Clinician Social Worker who has worked extensively in ED and PICU. Specialises in counselling children,families and staff impacted by loss, trauma, crisis and bereavement. Doing a PhD on Staff Wellbeing in Critical Care. Author of 'The Little Book of Loss and Grief You Can Read While You Cry'. Enjoys Gallows Humour. *Read Posts* | |||
 Dr Chris Gray BSc MBBS MRCP MRCEM Dr Chris Gray BSc MBBS MRCP MRCEMEmergency Medicine trainee at the Royal Manchester Children's Hospital. Interested in pre-hospital care, trauma, and critical care. Keen educator, musician and cake-maker. *Read Posts* | |||
 Ashley Liebig RN Ashley Liebig RNVet 101st Airborne combat medic. Flight Nurse & Helicopter Rescue Specialist. ECMO enthusiast. | |||
 Dr Laura Howard Dr Laura HowardJunior doctor in Virchester. Interested in mountain bikes, resuscitation, trauma and critical care. *Read Posts* | |||
 Mr Ross Fisher Mr Ross FisherConsultant Paediatric Surgeon at Sheffield Children's Hospital and Chairman of TARNlet. Visiting lecturer in Virchester and basically anywhere else that will pay bus fare. Owns more Moleskine notebooks than is healthy, most of them full of ideas on #presentationskills Passionate convert to all things #FOAMy *Read Posts* | |||
 Dr Dan Horner BA, MBBS, MRCP, MCEM, FRCEM Dr Dan Horner BA, MBBS, MRCP, MCEM, FRCEMConsultant Emergency Physician at Salford Royal Hospitals Trust with subspecialty training in Intensive Care Medicine. Researcher with specialist interest in EBM and thromboembolic disease. New to all this blogging and tweeting, but old to the general chaos and lividity of the Emergency Department. An interest in VTE, Critical Care and a bit of trauma now and then. Also trying to stay sane while being overworked and underpaid. *Read Posts* |
Contributors
 Dr Gareth Hardy Dr Gareth HardyEmergency Medicine trainee with a long running and excellent blog. Thinks beyond the superficial and constantly questions the evidence for what we do.(Ed - A great asset and probably the only person here who knows what he's doing!) *Read Posts* | |||
 Dr Craig Ferguson FCEM Dr Craig Ferguson FCEMEmergency physician, Manchester Royal Infirmary. Interests in medical technology, resuscitation and medical research. Research interests in the diagnosis of acute heart failure in the ED. Fellow of the College of Emergency Medicine. *Read Posts* |

Monday May 15, 2017
Monday May 15, 2017
A critical appraisal nuggest on simple ways to understand the true effect of an intervention. Also see this more in depth podcast done with Iain Beardsell
http://ebem.podbean.com/2011/11/03/statistics-2/
vb
S

Sunday Mar 05, 2017
Ep 89 - March 2017 Round Up
Sunday Mar 05, 2017
Sunday Mar 05, 2017
In a new podcast format Simon (@EMManchester) and Iain (@docib) discuss the month's offerings from the St Emlyn's blog and podcast (www.stemlynsblog.org).
It's been a month full of interesting posts on subjects as diverse as Thrombolysis in Stroke (Alan Grayson), The Future of Emergency Medicine in the Social Age (Simon), Cardiac Arrest Centres (Simon), Love in Critical Care (Liz Crowe), Transfers (Nat and Simon), Thrombolysis in PE (a guest post from FOAMed legend Anand Swarminathan) and Benzos in Back Pain (Janos). Head to the website for the articles themselves and all the references and links you need.
We're aiminig to make this a regular monthly podcast - let us know if it's useful and enjoyable and how we could make it even more educational.

Saturday Jan 14, 2017
Ep 87 - Critical Appraisal Nugget 6: Retrospective and Prospective studies
Saturday Jan 14, 2017
Saturday Jan 14, 2017
Understanding Prospective and Retrospective Studies: Key Differences, Advantages, and Applications
In the field of medical research, the distinction between prospective and retrospective studies is fundamental. These study designs differ primarily in the timing of data collection relative to the occurrence of outcomes, which significantly influences the quality, reliability, and applicability of the research findings. This detailed exploration aims to elucidate the characteristics, strengths, and limitations of each design, offering practical insights into their use in clinical research and practice.
Defining Prospective and Retrospective Studies
Prospective Studies involve the identification and enrollment of participants before the outcomes of interest occur. This design allows researchers to follow participants over time, observing events as they happen. For instance, in a study focused on chest pain, researchers would enrol patients at the onset of symptoms and monitor them to see if they develop conditions like myocardial infarction (MI). The prospective nature of these studies provides a structured approach to data collection, ensuring that all relevant information is captured consistently.
Retrospective Studies, conversely, involve examining existing data after the outcomes have occurred. In this design, researchers typically review medical records or databases to identify patients who have experienced specific events, such as an MI, and then analyze these records to explore potential risk factors or causes. This approach is often more efficient and less costly than prospective studies, as it utilizes data that have already been collected.
Key Differences Between Prospective and Retrospective Studies
The timing of data collection in relation to the occurrence of outcomes is a critical differentiator between these study designs. This temporal aspect influences several key factors, including data quality, potential biases, and the strength of causal inferences that can be drawn.
Data Collection and Quality
One of the primary advantages of prospective studies is the ability to standardize data collection. Since the data is collected in real-time, researchers can establish clear protocols for what data to collect and how to collect it. This reduces variability and enhances the reliability of the study findings. For example, in a prospective study on hypertension, researchers can use a standardized checklist to document whether each participant has hypertension, ensuring consistent and accurate data across all participants.
In contrast, retrospective studies depend on the quality and completeness of existing records, which were often not compiled with the current research question in mind. This reliance on historical data can lead to inconsistencies and gaps. For instance, a patient's medical record might not specify whether they had hypertension, either because it was not asked about or not documented. Such missing data can lead to biases and affect the study's conclusions, as the researchers may not have all the necessary information to make accurate assessments.
Timing and Outcome Identification
In prospective studies, participants are observed from the point of exposure or initial symptoms to the outcome, allowing researchers to track changes over time and potentially identify causative factors. This direct observation of the sequence of events enhances the ability to establish a cause-and-effect relationship. For instance, if a prospective study monitors patients presenting with chest pain, it can track the development of MI, thereby strengthening the evidence for an association between initial symptoms and outcomes.
Retrospective studies, however, start with the outcome and work backwards to explore potential causes. This backwards-looking approach can introduce recall bias and selection bias, as the outcomes are already known and may influence which data are emphasized or selected. Additionally, retrospective studies are constrained by the availability and accuracy of past records, which can vary widely and may not cover all variables of interest, potentially leading to incomplete or skewed data.
Advantages and Limitations of Each Study Design
Both prospective and retrospective studies offer unique benefits and face distinct challenges, making them suitable for different types of research questions and practical considerations.
Prospective Studies
Advantages:
- High Data Quality: Prospective studies allow for systematic and standardized data collection, minimizing the risk of missing or incomplete data.
- Causal Inference: The temporal relationship between variables and outcomes can be clearly established, supporting stronger causal inferences.
- Real-Time Data Collection: Researchers can monitor the study as it progresses, allowing for adjustments to data collection methods if new relevant variables emerge.
Limitations:
- Resource-Intensive: Prospective studies often require significant time, financial investment, and effort. The need for long-term follow-up can be particularly demanding.
- Long Duration: These studies can take years to complete, especially for conditions with long latency periods, delaying the availability of results.
- Participant Dropout: Over extended periods, there is a higher risk of participant dropout, which can reduce the study's validity and potentially bias the results.
Retrospective Studies
Advantages:
- Efficiency: Retrospective studies can be conducted relatively quickly since they rely on already available data.
- Lower Cost: The use of existing records reduces the need for expensive data collection processes, making these studies more cost-effective.
- Feasibility for Rare Conditions: Retrospective studies are particularly useful for examining rare conditions or outcomes that would require a prohibitively large cohort in a prospective design.
Limitations:
- Data Quality Issues: Relying on existing records can lead to inconsistent data quality, with gaps or inaccuracies potentially affecting the study's findings.
- Bias: These studies' retrospective nature can introduce biases, such as selection bias and information bias, that can compromise the validity of the results.
- Limited Causal Inference: Establishing a cause-and-effect relationship is more challenging due to the lack of temporal clarity between exposure and outcome.
Practical Application in Medical Research and Practice
Understanding the strengths and weaknesses of prospective and retrospective studies is essential for effectively interpreting medical literature and applying research findings in clinical settings. For example, a study evaluating the effectiveness of a diagnostic tool for acute coronary syndrome would be assessed differently depending on whether it was conducted prospectively or retrospectively.
Prospective studies are often regarded as the gold standard for clinical trials, particularly when testing new treatments or interventions. Their ability to minimize bias and control for confounding variables makes them invaluable for determining efficacy and safety. However, the high cost and time requirements can be significant barriers, especially in large-scale studies or those requiring long-term follow-up.
While not as robust in establishing causality, retrospective studies are highly valuable for exploring existing data and generating hypotheses. They are especially useful in situations where prospective studies are impractical due to ethical concerns, time constraints, or the rarity of the condition being studied. For instance, retrospective analyses of patient records can provide insights into the natural history of a disease or the effectiveness of treatments in real-world settings.
Case Study: Evaluating the HEART Score
The HEART score, a tool used in emergency departments to risk stratify patients with chest pain, serves as an illustrative example of the application of these study designs.
In a prospective study, researchers would enrol patients presenting with chest pain and systematically apply the HEART score, following these patients over time to track outcomes such as MI or other adverse cardiac events. This prospective approach allows for a controlled and consistent application of the score, with data collected in real time. Researchers can ensure that all relevant factors, such as patient history and troponin levels, are accurately recorded, providing a clear picture of the score's predictive value.
In a retrospective study, researchers might review existing medical records of patients who presented with chest pain and were tested for troponins. They would calculate the HEART score based on the available data and correlate it with documented outcomes. While this method is more efficient and cost-effective, it is limited by the quality of the records. Incomplete or inaccurately recorded data, such as missing details on patient history, can affect the accuracy of the HEART score's evaluation, potentially leading to less reliable conclusions.
Ethical Considerations
Ethical considerations differ significantly between prospective and retrospective studies. Prospective studies often require informed consent from participants, as they involve collecting new data. This process ensures that participants are aware of the study's purpose, procedures, and potential risks, and they have the right to withdraw at any time. However, obtaining consent can be challenging in emergency settings or when the study involves vulnerable populations.
Retrospective studies typically use anonymized data, which simplifies ethical considerations by removing the need for consent. This approach is particularly advantageous when dealing with sensitive information, as it protects patient privacy and confidentiality. However, researchers must still ensure that data are used responsibly and that individuals' privacy is not compromised. The use of anonymized data also limits the ability to collect additional information that may be relevant to the study but was not included in the original records.
Conclusion: Choosing the Right Study Design
The decision between using a prospective or retrospective study design should be guided by the research question, available resources, and the specific context of the study. Each design offers unique benefits and challenges, and the choice will impact the strength and applicability of the findings.
Prospective studies are preferred when high-quality data and strong causal inferences are needed, despite their higher costs and time requirements. They are ideal for intervention studies, where controlling for confounding factors is crucial.
While limited in establishing causality, retrospective studies provide valuable insights when prospective studies are not feasible. They are particularly useful for exploring existing data, understanding the epidemiology of diseases, and identifying potential risk factors.
In clinical practice, understanding these differences helps healthcare professionals critically appraise the literature, making informed decisions based on the strengths and limitations of the evidence. At St Emlyn's, we emphasize the importance of critical appraisal and evidence-based practice. By familiarizing yourself with these study designs, you can enhance your ability to interpret research findings, apply them in clinical settings, and contribute to the ongoing advancement of medical knowledge.
Thank you for exploring the complexities of prospective and retrospective studies with us. We hope this detailed discussion has provided clarity and practical guidance, empowering you to approach medical research with a critical and informed perspective. For more in-depth analysis and practical insights, continue following St Emlyn's, your trusted source for cutting-edge medical education and research.

Thursday Nov 17, 2016
Ep 83 - The Teaching Course in NYC Round Up
Thursday Nov 17, 2016
Thursday Nov 17, 2016
Insights from the New York Teaching Course: Enhancing Medical Education
Welcome to the St. Emlyn's blog! I'm Iain Beardsell, sharing insights from the recent New York Teaching Course, an event organized by Rob Rogers and Saline Rissai. This course brought together educators from diverse backgrounds, including pediatric surgeons, flight nurses, PhD students, and even a veterinarian, all united by the goal of becoming better educators. Notable attendees included Ross Fischer, Ashley Leibig, Sandra Viggers, and Camilla Sauronson, who shared their experiences and key takeaways.
Diverse Expertise and Shared Learning
The New York Teaching Course offered a unique opportunity to learn from a broad spectrum of expertise. Ross Fischer, a Pediatric Surgeon and presentation expert, found it humbling to be sought after for his advice on presentation skills. He highlighted the importance of continual improvement, noting the evolution of presentations over the years. His blog, ffoliet.com, offers valuable tips for enhancing presentation skills, a crucial aspect of effective teaching.
Ashley Leibig, known for her contributions to St. Emlyn's and her work at SMAC, emphasized the value of open communication. She appreciated the honesty in feedback sessions, where participants openly shared their past errors and positive feedback practices. This openness is essential for professional growth and creating a safe learning environment.
Sandra Viggers, a research fellow at the Copenhagen Academy for Medical Education and Simulation, focused on the power of vulnerability in simulation and debriefing. She found the social events particularly impactful, highlighting a moment where a participant shared a personal story, moving many to tears. This reinforced the importance of sharing and building a supportive community in educational settings.
Camilla Sauronson, a medical student from Denmark and PhD candidate in Tourette Syndrome, valued the inspiring environment of the course. She was particularly interested in innovative teaching methods like the flipped classroom, which involves engaging learners with materials before group discussions. This method fosters active learning and deeper understanding, a shift from traditional lecture-based teaching.
Key Takeaways and Learning Points
The course provided numerous valuable insights and practical lessons:
-
Flipped Classroom: Camilla Sauronson emphasized the effectiveness of the flipped classroom approach, which encourages students to engage with educational content before attending group discussions. This method promotes active learning and enriches classroom interactions.
-
Constructive Feedback: The feedback session led by George Willis was a highlight, demonstrating the importance of giving constructive feedback. Ashley Leibig noted the challenges in providing good feedback but appreciated the practical pointers provided during the session. Effective feedback is critical for personal and professional development.
-
Presentation Skills: Ross Fischer underscored the continuous need to refine presentation skills. His insights into slide design and delivery were invaluable, reminding educators of the importance of clear and engaging communication in teaching.
-
Resilience and Wellbeing: Sandra Viggers reflected on Chris Doty's talk on resilience. Doty discussed recognizing signs of burnout and the importance of self-care. Sandra emphasized the need for educators to be mindful of their own and their learners' wellbeing, highlighting the role of supportive relationships in preventing burnout.
-
Engaging Lectures: Ken Mills' interactive workshop on evidence-based medicine showcased that lectures can be both educational and entertaining. Using historical figures to illustrate concepts made the session memorable and engaging, demonstrating that education can and should be enjoyable.
Building a Supportive Educational Community
A particularly poignant moment during the course was a participant sharing a deeply personal story during a social event. Sandra Viggers emphasized the significance of vulnerability and the supportive community fostered at the course. This sense of community is vital in emergency medicine and education, where the pressures of the job can be intense. Building strong, supportive networks helps individuals navigate challenges and grow both personally and professionally.
Practical Applications and Future Directions
As the course concluded, participants were encouraged to apply what they had learned in their own teaching practices. Key practical steps include:
- Implementing the Flipped Classroom: Start by incorporating pre-session materials like podcasts or articles, fostering richer discussions during group sessions.
- Developing Effective Feedback Techniques: Create a structured approach to giving feedback, focusing on being constructive and empathetic.
- Enhancing Presentation Skills: Regularly review and improve presentation materials, seeking feedback from peers.
- Prioritizing Wellbeing: Integrate wellbeing discussions into educational curricula and encourage self-care practices among staff and students.
- Fostering a Supportive Community: Create opportunities for personal sharing and team-building, strengthening trust and collaboration.
Looking Forward
The New York Teaching Course was an enriching experience, and similar events are planned for the future, including one in Copenhagen before the next SMAC conference. These courses provide more than just educational content; they are opportunities to connect with a global community of educators dedicated to improving their craft.
For more detailed reflections and session summaries, the Scan FOAM website offers comprehensive coverage. Their posts provide a virtual experience of the course, nearly as immersive as attending in person.
Conclusion: A Commitment to Continuous Improvement
The New York Teaching Course reinforced that teaching is not merely about imparting knowledge but about connecting with students, being vulnerable, and continuously improving. Whether you're an experienced educator or just starting, there's always room for growth. Let's carry forward the lessons learned, strive to be better educators, and support our students and colleagues. Thank you for joining us on this journey, and stay tuned for more insights and stories from St. Emlyn's. Keep learning, keep teaching, and be the best educator you can be.
Sunday Jul 31, 2016
Sunday Jul 31, 2016
Effective Trauma Handovers: Best Practices and Key Considerations
Trauma handovers are critical transitions in patient care, transferring responsibility from pre-hospital teams to in-hospital teams. These moments are crucial for ensuring patient safety and the continuation of effective treatment. This summary explores the best practices for trauma handovers, focusing on preparation, timing, communication, and the integration of feedback.
Preparation: Utilizing Golden Time
Effective trauma handovers begin with thorough preparation. The period between receiving the notification of an incoming trauma patient and their arrival is often called "golden time." This time should be used to organize and prepare the multidisciplinary team, including in-patient specialists, ED staff, nurses, doctors, and radiologists. Key preparatory steps include:
- Role Allocation: Assign clear responsibilities, such as the trauma team leader, scribe, airway manager, and primary survey conductor. It is crucial to ensure that team members are both competent and confident in their assigned roles, as these attributes, while related, are distinct.
- Predictive Planning: Use pre-hospital information to anticipate the patient's needs. For instance, a report of a patient with a chest stab wound and hypotension suggests the need to prepare for a thoracotomy.
Timing and Coordination
Timing is essential in trauma care, particularly in avoiding early calls to the trauma team. At Southampton, the recommended practice is to call the team together approximately 15 minutes before the patient’s expected arrival, avoiding exact time estimates. This strategy helps maintain team readiness and focus. The risks of early calls include loss of focus due to prolonged waiting and the potential for team members to become distracted by other tasks.
Conducting the Team Briefing
A comprehensive and unified briefing is vital upon the trauma team’s assembly. This briefing should involve the entire multidisciplinary team, preventing any division into subgroups and ensuring that all members receive the same information. A good practice is for team members to introduce themselves using first names, which helps break down hierarchical barriers and fosters a collaborative environment. The briefing should also include a mission rehearsal, outlining the specific tasks and roles each member will perform upon the patient's arrival.
The Handover Process
The actual handover begins when the patient arrives. The in-hospital team leader should introduce themselves to the pre-hospital team and determine if the patient is stable enough for a hands-off handover. This approach, modeled after military practices, ensures that the handover is conducted calmly and clearly. If the patient is unstable, the pre-hospital team should continue leading the resuscitation until it is safe to hand over control.
A structured framework, such as AppMist (Age, Time of injury, Mechanism, Injuries, Signs, and Treatments), should be used to deliver concise and critical information during the handover. This approach ensures that only the essential information is communicated, focusing on the most pertinent details for the ongoing treatment.
Addressing Pre-Hospital Challenges
The pre-hospital environment is inherently stressful and challenging, with limited resources and a high cognitive load. Pre-hospital teams often face the dual pressures of managing critically ill patients and communicating effectively with the receiving hospital. It is crucial for in-hospital teams to recognize these challenges and refrain from criticizing or undermining pre-hospital efforts during the handover. Instead, the focus should be on receiving and clarifying the necessary information to continue patient care.
Pre-hospital teams should aim to deliver concise, relevant information during the handover. Ending the handover with a clear statement, such as "That completes my handover," followed by an offer to answer any urgent questions, helps ensure clarity and completeness.
Feedback and Continuous Improvement
Closing the feedback loop is an essential aspect of improving trauma care. Providing feedback to pre-hospital teams about patient outcomes helps refine their assessment and treatment strategies. This feedback should be delivered sensitively, acknowledging the emotional and high-pressure nature of pre-hospital work.
Constructive feedback should focus on confirming or refuting pre-hospital assessments and decisions, providing a learning opportunity for future cases. It is essential to approach feedback with empathy and professionalism, fostering a supportive environment for continuous improvement.
Controversial Aspects and Best Practices
Calling the Full Trauma Team: There is a debate over whether to always call the entire trauma team for every alert. At our hospital, we favor over-calling to ensure that all necessary resources are immediately available, even if it means releasing some staff after assessing the situation.
Pre-Hospital Requests for Specific Interventions: In-hospital teams must use their discretion when responding to pre-hospital requests for specific interventions or specialist involvement. Trust and familiarity with the pre-hospital team's capabilities influence these decisions. For example, while cardiothoracic surgeons are not standard members of our trauma team, they may be involved in cases of traumatic cardiac arrest with penetrating trauma.
Conclusion: A Framework for Effective Trauma Handover
Effective trauma handovers are essential for patient safety and optimal care. This process requires careful preparation, clear communication, and seamless coordination between pre-hospital and in-hospital teams. By adhering to standardized practices, fostering a collaborative environment, and integrating constructive feedback, healthcare providers can significantly enhance the quality of trauma care.
We encourage healthcare professionals to share their experiences and insights, contributing to a broader understanding of best practices in trauma handovers. Whether you are working in trauma centers, units, or in different healthcare systems worldwide, your input is invaluable in refining these critical processes.
Thank you for engaging with this discussion on the St Emlyns blog. We look forward to continuing this conversation and exploring ways to improve patient care in emergency medicine.

Friday Jul 08, 2016
Friday Jul 08, 2016
Enhancing Pre-Hospital to Hospital Handover: Insights from SMACC Dublin
The SMACC Dublin conference provided a valuable platform for discussing the crucial handover process from pre-hospital teams to hospital staff. This transition is essential for patient safety and continuity of care, as it involves conveying critical information from emergency responders to hospital-based healthcare professionals. The discussion at the conference highlighted several key issues, best practices, and strategies to improve this critical interface.
The Emotional Landscape and Communication Challenges
Dr. Natalie May, reflecting on her shift from hospital to pre-hospital care, emphasized the emotional challenges and the need for empathy and understanding between both teams. Pre-hospital providers often face a tense environment upon hospital arrival, with varying degrees of reception from the hospital team. This tension can arise from perceived disrespect or a lack of understanding of the pre-hospital team's challenges, which can complicate the handover process.
A significant issue in handover is the lack of structured communication. The fast-paced environment of the emergency department (ED) can pressure pre-hospital providers to quickly pass on patients and information, sometimes resulting in incomplete or rushed handovers. To address this, the use of structured communication tools like the AD MISSED acronym (Age, Date/Time, Mechanism of Injury, Injuries, Signs/Symptoms, Treatments, and Decisions) was recommended. This structure helps ensure that all essential information is conveyed systematically, minimizing the risk of information loss.
Best Practices for Handover
One highlighted best practice is the implementation of a clear and consistent protocol. For instance, a Texas hospital has adopted a "hands-off" period during handover, where the receiving team does not intervene until the pre-hospital team has completed their report. This approach helps maintain focus on the verbal communication of critical details without distractions, ensuring a comprehensive transfer of information.
The role of the trauma team leader is also critical. They act as the primary point of contact, receiving the handover and ensuring that all relevant team members understand the conveyed information. The trauma team leader is responsible for verifying the accuracy of the information, clarifying any uncertainties, and coordinating subsequent actions. This leadership role is crucial in maintaining a smooth and efficient handover process.
Overcoming Communication Barriers
Differences in communication styles and preferences between hospitals can pose challenges. The discussion emphasized the need for pre-hospital teams to be adaptable, potentially rehearsing handovers and using aids like whiteboards. Regular joint training sessions between pre-hospital and hospital teams were recommended to align expectations and familiarize each side with the other's protocols. The use of digital tools, such as secure messaging apps, can also facilitate better communication and continuity of care.
The physical environment during handover significantly impacts its effectiveness. A calm, organized setting with minimal interruptions is ideal for ensuring a thorough transfer of information. Designating a specific area for handovers and equipping it with necessary tools, such as a whiteboard and a scribe, can improve the clarity and accuracy of the communication.
The Importance of Feedback
Immediate feedback after handover is crucial for continuous improvement. It allows pre-hospital providers to understand the outcomes of their interventions and the patient's progression. This real-time feedback can highlight areas for protocol refinement and training. Additionally, formal long-term feedback mechanisms, such as follow-up meetings or debriefings, are vital for providing a complete picture of the patient's journey, helping both pre-hospital and hospital teams improve their practices.
Building a Culture of Respect and Understanding
A successful handover process is built on mutual respect and understanding between pre-hospital and hospital teams. Acknowledging the expertise and challenges faced by each group fosters a more cooperative and supportive environment. This respect is essential for enhancing patient care and ensuring a smooth transition from one care setting to another.
To build this culture of respect, regular interdisciplinary workshops and social events can help break down barriers and build rapport among healthcare professionals. Recognizing the unique pressures and responsibilities of each team member contributes to a more harmonious and effective handover process.
Conclusion: Towards a Seamless Continuum of Care
The discussions at SMACC Dublin underscored the importance of an effective handover in emergency medicine. By adopting structured communication protocols, ensuring clear leadership, and fostering a culture of continuous feedback and mutual respect, the gap between pre-hospital and hospital care can be bridged. The ultimate goal is to create a seamless continuum of care, where the transition between healthcare teams is smooth, efficient, and centered on the patient's best interests.
This integrated approach not only improves patient outcomes but also enhances job satisfaction among healthcare providers by reducing miscommunications and misunderstandings. The handover process is a critical component of patient care that requires ongoing attention and improvement.
In conclusion, effective handover practices are essential for ensuring patient safety and continuity of care. The insights from SMACC Dublin provide valuable guidance on refining these practices. By fostering a culture of learning, respect, and collaboration, healthcare providers can ensure that every patient transition is handled with the utmost professionalism and care.

Wednesday Dec 09, 2015
Ep 61 - Londoon Trauma Conference 2015 Day 2 Summary
Wednesday Dec 09, 2015
Wednesday Dec 09, 2015
Our summary of Day 2 of the excellent London Trauma Conference. A unique threesome from Nat, Simon and Iain.....

Tuesday Dec 08, 2015
Ep 60 - Londoon Trauma Conference 2015 Day 1 Summary
Tuesday Dec 08, 2015
Tuesday Dec 08, 2015
Greetings from the London Trauma Conference!
As has become our pre-Christmas custom, Iain and I have been hanging out at the fabulous London Trauma Conference, hearing about advances and controversies in trauma care and tracking down some of the speakers to find out exactly what they really think (and recording it, for podcasts we'll release in due course).
The conference extends over four days, incorporating the Air Ambulance and Prehospital Day and the Cardiac Arrest Symposium; unfortunately we can't stick around for those but our colleagues over at the RCEM FOAM network will be podcasting from those days too, so keep an eye on their site and podcast feed too.

Saturday Nov 28, 2015
Ep 58 - Clinical Judgement for the Emergency Physician
Saturday Nov 28, 2015
Saturday Nov 28, 2015
My talk from the RCEM conference in Manchester 2015.
Linked blog post here. http://stemlynsblog.org/making-good-decisions-in-the-ed-rcem15/
Slides are here http://www.slideshare.net/simoncarley7/making-good-decisions-rcem-2015-manchester-wednesday
Have fun and enjoy your emergency medicine.
S

Thursday Jun 04, 2015
Ep 48 - Intro to EM: The patient with back pain.
Thursday Jun 04, 2015
Thursday Jun 04, 2015
Managing Back Pain in the Emergency Department: A Comprehensive Overview
In the emergency department (ED), back pain, particularly lower back pain without a traumatic cause, is a common and complex presentation. This condition can range from benign to life-threatening, requiring a thorough and systematic approach to ensure accurate diagnosis and effective management.
The Challenge of Back Pain in Emergency Medicine
Back pain patients often come with preconceived notions, especially when they seek pain relief. However, it's crucial to avoid jumping to conclusions, as back pain can result from various underlying issues, including serious conditions like ruptured abdominal aortic aneurysms (AAA) or infections. Therefore, clinicians should avoid hastily labeling cases as "musculoskeletal" without thorough evaluation.
Key Diagnostic Considerations
1. Broad Differential Diagnosis:
The differential diagnosis should begin with more severe and potentially life-threatening conditions. For example, an AAA can present with subtle back pain, particularly in the elderly, and missing this diagnosis can be catastrophic. Hence, abdominal examinations and bedside ultrasounds are essential tools for detection.
2. Pain Chronology and Characteristics:
Understanding the pain's duration and nature is vital. Chronic pain may suggest long-standing issues, while acute pain can indicate new, potentially severe conditions. Atypical symptoms like pain that worsens at night or at rest, as opposed to musculoskeletal pain that improves with rest, could signal neoplastic or infectious processes.
3. Multi-System Evaluation:
A comprehensive assessment, including vital signs and a review of systems, is critical. For instance, signs like tachycardia, fever, or hypotension can indicate systemic issues such as sepsis. Conditions like pyelonephritis, especially in immunocompromised patients, can manifest as back pain, necessitating a thorough evaluation.
Specific Conditions and Red Flags
Ruptured Abdominal Aortic Aneurysm (AAA):
In elderly patients, AAA must always be considered, especially with sudden onset back pain. This condition can be rapidly fatal, and quick diagnosis via ultrasound is crucial.
Neoplastic Disease:
Symptoms such as unexplained weight loss, persistent night pain, or a history of cancer necessitate evaluation for metastatic disease. Cancers known to metastasize to bone, like breast or lung cancer, may present with back pain, requiring thorough imaging and lab work.
Infectious Causes:
Spinal infections, such as osteomyelitis or epidural abscess, are serious conditions often presenting with back pain. Risk factors include intravenous drug use or immunocompromised states. High suspicion is necessary in patients with concurrent systemic symptoms.
Cauda Equina Syndrome (CES):
CES is a neurosurgical emergency, presenting with symptoms like severe lower back pain, saddle anesthesia, and bowel or bladder dysfunction. A meticulous neurological examination, focusing on lower limb function and perineal sensation, is necessary. MRI is the preferred diagnostic tool, providing detailed images of the spinal cord and nerve roots.
Imaging and Laboratory Tests
Imaging:
Imaging choices should be guided by clinical suspicion. MRI is preferred for evaluating soft tissues, especially in suspected CES cases. For older adults, plain X-rays can reveal fractures but are limited in detecting soft tissue issues. CT scans are useful for complex cases like suspected tumors or infections, while nuclear medicine imaging may detect metastatic lesions or stress fractures.
Laboratory Tests:
Blood tests are essential in cases where red flags suggest systemic involvement. Tests like a full blood count (FBC), inflammatory markers, and bone profiles can provide critical diagnostic information. Elevated inflammatory markers may indicate infection or inflammation, while abnormal calcium levels could suggest a paraneoplastic syndrome.
Management of Non-Specific Back Pain
Once serious conditions are ruled out, management focuses on non-specific, likely musculoskeletal back pain. This involves patient education, mobilization, and appropriate pain management.
Patient Education and Mobilization:
Patients should be informed about the importance of staying active to prevent muscle stiffness and worsening pain. The role of muscle spasm in pain should be explained, and patients encouraged to maintain activity despite discomfort.
Pain Management:
The WHO pain ladder guides pain management, starting with simple analgesics like paracetamol and NSAIDs. For more severe pain, moderate opioids like codeine may be considered. The goal is to provide sufficient pain relief to facilitate mobilization and prevent the development of chronic pain.
Controversial Treatments:
The use of benzodiazepines is controversial. They are not true muscle relaxants but can reduce anxiety and distress, potentially aiding pain management. However, they should be used sparingly and for short periods. The use of gabapentin for acute back pain is also debated, as it is primarily indicated for neuropathic pain.
Chronic Pain Management
For chronic pain patients, management focuses on a multidisciplinary approach, involving pain specialists, physiotherapists, and primary care providers. The goal is to manage the physical, psychological, and social aspects of chronic pain.
Collaborative Care:
Close collaboration with primary care providers ensures consistent messaging and management plans. Pain specialists can offer additional support, especially in complex cases requiring advanced pain management techniques.
Non-Pharmacological Interventions:
Non-pharmacological interventions, such as physical therapy and cognitive-behavioral therapy (CBT), are crucial. These therapies help strengthen muscles, improve posture, and manage the psychological impacts of chronic pain.
Conclusion
In conclusion, managing back pain in the ED requires a comprehensive, systematic approach. Clinicians must prioritize ruling out serious conditions, use appropriate diagnostic tools, and provide effective pain management and patient education. Collaboration with primary care and pain specialists is essential for managing chronic pain, ensuring a holistic approach to patient care. By following these guidelines, healthcare professionals can provide compassionate, evidence-based care, leading to better patient outcomes and a more efficient emergency department.
Red flag symptoms and analgesia advice below.
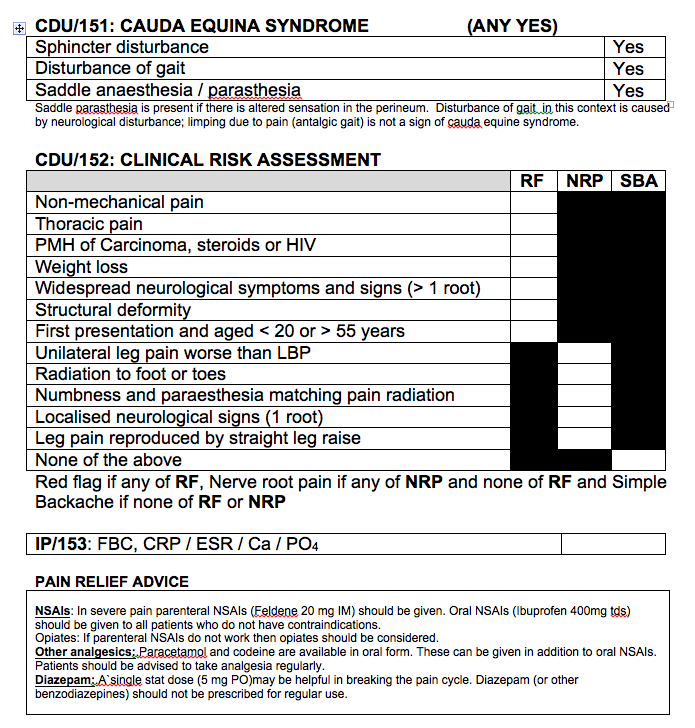

Saturday Apr 18, 2015
Ep 44 - Tim Draycott on Obstetric Trauma (LTC 2014)
Saturday Apr 18, 2015
Saturday Apr 18, 2015
Iain interviews the wonderful Tim Draycott on the management of the Obstetric patient with trauma.Tim is a consultant Obstetrician from Bristol and is a great speaker on this rather terrifying topic!

Thursday Mar 26, 2015
Ep 43 - APLS 2015 updates for the management of the serious injured child
Thursday Mar 26, 2015
Thursday Mar 26, 2015

A short podcast updating the UK Advanced Paediatric Life Support (APLS) course guidelines for the management of trauma in children.
Don't forget to read the blog post here. APLS Updates: New kids on the block,
vb
S
Sunday Mar 22, 2015
Ep 42 - Paediatric Major Trauma with Ross Fisher (LTC 2014)
Sunday Mar 22, 2015
Sunday Mar 22, 2015
Title: Rethinking Pediatric Trauma: Insights from the London Trauma Conference
Welcome to another insightful post from St Emlyns, where we dive into the latest discussions and research in emergency medicine. In this post, we recap a conversation with Rosfisher, a pediatric surgeon from Sheffield, who recently presented at the London Trauma Conference. Rosfisher shared his perspectives on pediatric trauma management, the challenges of research in this field, and the art of effective presentation. Let's explore these critical topics and their implications for emergency care.
Pediatric Trauma: A Unique Challenge
Pediatric trauma is an infrequent yet crucial area in emergency medicine, necessitating a distinct approach. Rosfisher emphasized that children are not simply "small adults." This fundamental concept underlines the need for specialized knowledge and skills when managing pediatric trauma. Despite the rarity of severe pediatric trauma cases, healthcare professionals must understand that children's anatomical, physiological, and pathological differences require tailored treatment strategies.
Understanding the Differences
One of the key points Rosfisher highlighted is the unique nature of pediatric anatomy and physiology. Unlike adults, children have different injury patterns, and their bodies respond differently to trauma. This distinction is crucial for emergency physicians, pediatric surgeons, and anesthetists, who must adjust their standard protocols to suit pediatric needs. The importance of recognizing these differences cannot be overstated, as it directly impacts the outcomes of pediatric trauma cases.
The Debate on FAST Scanning in Pediatric Trauma
A significant portion of Rosfisher's discussion focused on the use of Focused Assessment with Sonography for Trauma (FAST) in pediatric cases. While FAST scanning is a well-established practice in adult trauma, its efficacy in pediatric patients remains controversial. Rosfisher pointed out the lack of robust evidence supporting the reliability of FAST scans in children, citing a 50% sensitivity and specificity rate—equivalent to flipping a coin.
Limitations and Concerns
The concerns surrounding FAST scanning in pediatric trauma revolve around its diagnostic accuracy and the subsequent decision-making process. Rosfisher noted that even if healthcare professionals are skilled in using FAST scans on adults, this expertise does not necessarily translate to pediatric patients. The anatomical and physiological differences mean that the interpretation of FAST scans in children is more complex and less reliable. As a result, the decisions based on these scans carry a high risk of error.
The Role of CT Scans
In light of the limitations of FAST scanning, Rosfisher advocated for the use of computed tomography (CT) scans for pediatric blunt abdominal trauma. He referenced guidelines from the Royal College of Radiology, which recommend CT scans as the gold standard for imaging in these cases. The higher accuracy and reliability of CT scans make them a preferable option, providing clearer insights into the child's condition and guiding appropriate treatment.
Challenges in Pediatric Trauma Research
Pediatric trauma research is significantly underrepresented compared to adult trauma research. Rosfisher highlighted the stark contrast in research volume, with pediatric studies comprising less than half a percent of the total trauma research. This disparity poses a considerable challenge, as the lack of data hampers the development of evidence-based practices in pediatric trauma care.
Barriers to Research
Several factors contribute to the limited research in pediatric trauma. One major issue is the misconception that pediatric trauma is simply a scaled-down version of adult trauma. This oversimplification overlooks the complexities unique to children and the necessity for dedicated research in this area. Additionally, the relatively low incidence of pediatric trauma cases can make it difficult to conduct large-scale studies, further limiting the available data.
Opportunities for Growth
Despite these challenges, there is significant potential for growth in pediatric trauma research. The emergence of pediatric emergency medicine as a specialized field offers new avenues for research and development. Networks like PERUKI (Pediatric Emergency Research in the UK and Ireland) provide platforms for collaboration and innovation, encouraging more healthcare professionals to engage in pediatric trauma research.
Enhancing Presentation Skills in Medicine
Beyond his expertise in pediatric trauma, Rosfisher is passionate about improving presentation skills within the medical community. He argues that the way information is presented can significantly impact its retention and application. Many presentations, despite being rich in content, fail to leave a lasting impression due to poor delivery.
The Importance of Storytelling
Rosfisher advocates for incorporating storytelling into presentations. A well-structured narrative helps audiences follow the flow of information and retain key points. He uses the concept of an "arc of a story," similar to a plot in a film or book, to structure his talks. This approach ensures that the audience remains engaged and can easily recall the main message.
Practical Tips for Effective Presentations
For those looking to improve their presentation skills, Rosfisher offers several practical tips:
-
Know Your Content: Before delivering a talk, ensure you have a deep understanding of the subject matter. This foundation is essential for building a coherent and compelling presentation.
-
Elevator Pitch: Condense your talk into a brief "elevator pitch." If you can explain the essence of your presentation in 30 seconds, you are more likely to deliver a clear and focused message.
-
Audience Awareness: Tailor your presentation to your audience's needs and knowledge level. Understanding where your audience starts and where you want them to end up helps in crafting a relevant and impactful message.
-
Visual Aids: Use visuals to support your narrative. Rather than cluttering slides with text, use images and simple graphics that complement your spoken words and enhance understanding.
-
Consistency and Repetition: Start and end your presentation with the same message or visual cue. This technique reinforces the key takeaway and helps embed it in the audience's memory.
Case Study: Effective Use of Visual Aids
During his presentation at the London Trauma Conference, Rosfisher used several effective visual aids. He started and ended with the same video, challenging the audience to rethink their perspectives on pediatric trauma. He also employed a memorable device using the numbers 73 and 37, referencing the popular TV show "The Big Bang Theory." This consistent thread helped tie together various statistics and made the information more memorable for the audience.
Conclusion: A Call to Action in Pediatric Trauma
The insights shared by Rosfisher at the London Trauma Conference underscore the need for a nuanced approach to pediatric trauma. Recognizing that children are not small adults is a fundamental step in improving care and outcomes in this field. The discussions around the use of FAST scanning highlight the importance of evidence-based practices, while the challenges in pediatric trauma research call for greater investment and focus.
As healthcare professionals, it's crucial to continue exploring new methods and technologies, like CT scans, that can enhance diagnostic accuracy and treatment efficacy in pediatric cases. Moreover, by honing our presentation skills, we can ensure that vital knowledge and insights are effectively communicated, leading to better understanding and implementation of best practices.
In conclusion, pediatric trauma care requires a specialized approach, and the field offers numerous opportunities for research and innovation. We encourage our readers to engage with networks like PERUKI, contribute to research efforts, and continuously refine their skills, both in clinical practice and communication. Together, we can make significant strides in improving the care and outcomes for our youngest and most vulnerable patients.
Stay tuned for more insights and discussions from the St Emlyns blog, where we continue to explore the latest in emergency medicine and critical care. Don't forget to subscribe and follow us on social media for updates on our latest posts and podcasts.
Title: Rethinking Pediatric Trauma: Key Insights from the London Trauma Conference
In a recent discussion at the London Trauma Conference, Rosfisher, a pediatric surgeon from Sheffield, provided valuable insights into pediatric trauma care, the challenges of research in this field, and effective presentation techniques. This summary captures the key points from his presentations and discussions.
Pediatric Trauma: Understanding the Differences
Pediatric trauma presents unique challenges in emergency medicine. Rosfisher emphasized that children are not merely "small adults," a common misconception that can lead to inadequate care. The distinct anatomical, physiological, and pathological characteristics of children necessitate specialized approaches to treatment. Recognizing these differences is crucial for healthcare professionals, including emergency physicians, pediatric surgeons, and anesthetists, who must adjust their standard protocols accordingly.
The Controversy Around FAST Scanning
A significant portion of the discussion focused on the use of Focused Assessment with Sonography for Trauma (FAST) in pediatric cases. While FAST scanning is a well-established diagnostic tool in adult trauma, its efficacy in children is debatable. Rosfisher highlighted the lack of strong evidence supporting the reliability of FAST scans in pediatric trauma, citing a 50% sensitivity and specificity rate. This level of accuracy is akin to chance, making it a less reliable diagnostic tool for children.
The concern with FAST scanning lies not only in its accuracy but also in the potential consequences of basing clinical decisions on these results. Even experienced practitioners may struggle with interpreting FAST scans in children due to their distinct anatomical differences. As a result, there is a significant risk of incorrect decision-making. Rosfisher advocates for the use of computed tomography (CT) scans instead, as they offer more accurate and reliable imaging for pediatric blunt abdominal trauma. This recommendation aligns with guidelines from the Royal College of Radiology, which consider CT scans the gold standard in these cases.
Challenges in Pediatric Trauma Research
Research in pediatric trauma is significantly underrepresented compared to adult trauma research. Rosfisher pointed out that pediatric studies account for less than half a percent of all trauma research. This paucity of data presents a major challenge in developing evidence-based practices for pediatric trauma care. Several factors contribute to this lack of research, including the misconception that pediatric trauma is simply a scaled-down version of adult trauma and the relatively low incidence of severe pediatric trauma cases.
Despite these challenges, there is significant potential for growth in pediatric trauma research. The rise of pediatric emergency medicine as a specialized field offers new opportunities for research and innovation. Networks like PERUKI (Pediatric Emergency Research in the UK and Ireland) are fostering collaboration and encouraging more research in this area. Rosfisher emphasized the importance of starting with simple audit projects to assess current practices and gradually build a more comprehensive understanding of pediatric trauma care.
Improving Presentation Skills in Medicine
Beyond his expertise in pediatric trauma, Rosfisher is passionate about improving presentation skills within the medical community. He argues that the effective presentation of information is crucial for ensuring that important insights and knowledge are retained and applied. Often, the wisdom shared during medical presentations is lost due to poor delivery.
Rosfisher advocates for a storytelling approach in presentations. A well-structured narrative helps engage the audience and makes the information more memorable. He uses the concept of an "arc of a story," which involves structuring a presentation with a clear beginning, middle, and end, much like a film or book. This method helps the audience follow the flow of information and retain key points.
Practical Tips for Effective Presentations
Rosfisher offers several practical tips for improving presentation skills:
-
Master Your Content: Ensure a deep understanding of the subject matter. A technique like the "elevator pitch" can help distill the essence of a presentation into a concise summary, ensuring clarity and focus.
-
Audience Awareness: Tailor the presentation to the audience's knowledge level and interests. Understanding where the audience starts and where they should be by the end of the presentation is key to crafting an effective message.
-
Use of Visual Aids: Visuals should support the narrative rather than clutter the presentation with text. Images and simple graphics can enhance understanding and retention.
-
Consistency and Repetition: Using consistent themes and repeating key messages can reinforce the main points. For example, starting and ending a presentation with the same message or visual cue can help embed the information in the audience's memory.
Conclusion: A Call to Action in Pediatric Trauma
Rosfisher's insights highlight the need for a nuanced and specialized approach to pediatric trauma care. Recognizing the fundamental differences between children and adults is essential for providing appropriate treatment and improving outcomes. The debate around FAST scanning underscores the importance of evidence-based practices, while the challenges in pediatric trauma research call for increased focus and investment.
For healthcare professionals, engaging with research networks like PERUKI and contributing to pediatric trauma research are crucial steps toward advancing the field. Additionally, improving presentation skills can enhance the dissemination and retention of critical knowledge, leading to better clinical practices.
As we continue to explore and improve pediatric trauma care, we encourage our readers to stay engaged with ongoing research and professional development. Together, we can make significant strides in providing the best care for our youngest patients. Stay tuned for more insights and discussions from St Emlyns, where we continue to explore the latest in emergency medicine and critical care.

Friday Feb 27, 2015
Ep 40 - Opiate overdose in the ED
Friday Feb 27, 2015
Friday Feb 27, 2015
Managing Opiate Overdoses: Key Insights from St Emlyns
Opiate overdoses are a common and critical issue faced in emergency departments, especially in urban areas with prevalent drug use. This guide, based on insights from Dr. Simon Carley and Dr. Iain Beardsell, provides an in-depth look at recognizing, treating, and managing opiate overdoses, including potential complications and best practices for patient care.
Recognizing Opiate Overdoses
Patients present with opiate overdoses either accidentally or intentionally, including drug addicts, elderly patients overdosing on prescriptions, and those attempting self-harm. Recognizing an overdose involves identifying key symptoms:
- Depressed Level of Consciousness: Patients may appear lethargic or unresponsive.
- Respiratory Depression: A significantly reduced breathing rate.
- Myosis: Pinpoint pupils that are unresponsive to light.
- Cardiovascular Effects: In severe cases, patients may exhibit hypotension or bradycardia.
Initial Assessment and ABC Protocol
In cases of suspected opiate overdose, the initial assessment should follow the ABC (Airway, Breathing, Circulation) protocol:
- Airway: Ensure the airway is open and clear.
- Breathing: Assess and support breathing and ventilation as necessary.
- Circulation: Check for adequate blood pressure and oxygen saturation. Establish IV access for medication administration.
Administering Naloxone
Naloxone, an opiate antagonist, is the primary antidote for opiate overdoses. However, its administration must be cautious and titrated to avoid complications like acute withdrawal or revealing underlying conditions, such as stimulant overdoses.
Methods of Administration
- Intravenous (IV): Offers rapid onset, but should be administered in small aliquots (e.g., 100 micrograms) to prevent abrupt awakening and associated risks.
- Intramuscular (IM): Useful when IV access is challenging, though it has variable absorption rates.
- Intranasal (IN): Effective, especially in patients with adequate spontaneous respiration.
- Nebulized Naloxone: Useful for patients who are breathing but not fully responsive, allowing gradual titration.
Managing Long-Acting Opiates
Patients who have ingested long-acting opiates, such as methadone, require careful monitoring. Continuous naloxone infusion may be necessary to prevent re-sedation. The infusion rate should typically be two-thirds of the total dose needed to achieve the initial response.
Importance of Monitoring
Patients should be placed in a setting where continuous monitoring of ventilation can be performed. Suitable locations include:
- High Dependency Unit (HDU): For intensive monitoring.
- Acute Medical Unit (AMU): For stable patients needing continuous observation.
Advanced Monitoring Techniques
End-tidal CO2 monitoring can provide a continuous assessment of respiratory status, especially when high-flow oxygen is used, which can mask hypoventilation.
Addressing Concurrent Conditions
Opiate overdoses often coexist with other medical or substance-related conditions. Be vigilant for:
- Rhabdomyolysis: Caused by prolonged immobility, leading to muscle breakdown.
- Compartment Syndrome: Particularly in patients found unconscious for extended periods.
- Mixed Overdoses: Patients may also have ingested other substances like stimulants or tricyclic antidepressants, complicating treatment.
Psychosocial Considerations and Follow-Up
Patients presenting with opiate overdoses often have complex psychosocial needs. It is crucial to address these issues, including:
- Mental Health Assessment: Evaluate for deliberate self-harm and provide psychiatric support.
- Drug and Alcohol Services: Connect patients with support services for addiction.
- Homelessness Support: Involve homeless outreach teams as necessary.
Handling Recurrent Overdoses
It's not uncommon for patients to return with repeated overdoses, reflecting the chronic nature of addiction. While frustrating, healthcare providers must consistently offer support and care, recognizing that patients have autonomy in their choices.
Controversies and Emerging Practices
Recent case reports suggest potential benefits in ventilating hypercapnic, acidotic patients before administering naloxone to avoid complications like flash pulmonary edema or dysrhythmias. However, this practice remains controversial and requires careful risk-benefit analysis.
Case Study Insight
A notable case involved a pregnant patient with an opiate overdose who also had ingested cocaine and tricyclic antidepressants. Administering a high dose of naloxone precipitated severe withdrawal and unmasked the effects of other substances, leading to a critical situation. This highlights the importance of a controlled and gradual approach to naloxone administration.
Conclusion
Effective management of opiate overdoses in the emergency department requires a nuanced approach. This includes recognizing the signs, following the ABC protocol, and carefully administering naloxone. Continuous monitoring, addressing underlying conditions, and providing psychosocial support are crucial for comprehensive care. Stay informed on emerging practices and best practices to enhance patient outcomes. For more detailed guidelines and updates, follow the St Emlyns blog and join our discussions on emergency medicine best practices.

Sunday Feb 22, 2015
Ep 39 - Prof. Tim Harris on Shock Assessment (LTC 2014)
Sunday Feb 22, 2015
Sunday Feb 22, 2015
At the recent London Trauma Conference, Iain Beardsell from the St Emlyn's podcast interviewed Professor Tim Harris, an expert in Emergency Medicine at Bart's Health, who provided critical insights into the concept of shock. This discussion challenged traditional notions and emphasized the importance of understanding shock beyond simple metrics like blood pressure.
Redefining Shock: Beyond Blood Pressure
Professor Harris argued that shock should not be narrowly defined as a state of low blood pressure but rather as a condition of inadequate oxygen delivery to meet the body's needs. Traditional medical training often emphasizes measurable parameters such as pulse, blood pressure, and respiratory rate. However, these indicators do not fully capture a patient's physiological state, particularly the crucial aspect of cardiac output—the volume of blood the heart pumps per minute. Cardiac output is difficult to measure directly, especially in emergency settings, yet it is a vital determinant of whether a patient is experiencing shock.
Relying solely on blood pressure can be misleading. For instance, young, healthy individuals might maintain a systolic pressure of 80-90 mmHg while adequately perfusing their organs, whereas older patients with normally high blood pressure may experience organ dysfunction even with moderate drops in pressure. Therefore, a comprehensive assessment of shock must consider more than just blood pressure readings.
The Importance of Cardiac Output and Oxygen Delivery
A significant portion of the interview focused on the role of cardiac output and oxygen delivery. The body's oxygen needs vary based on physiological stressors such as physical activity or trauma. In trauma situations, patients often face substantial physiological stress, akin to "running for the bus," which increases their oxygen requirements. However, emergency assessments frequently emphasize visible signs like pulse and blood pressure, neglecting the more critical issue of oxygen delivery.
The traditional approach, which targets a specific blood pressure (often 90 mmHg systolic) as the threshold for shock, fails to account for individual differences in physiological response. For example, hypertensive patients with a baseline blood pressure of 200 mmHg may enter shock if their pressure drops to 120 mmHg. Conversely, young and fit individuals may tolerate much lower pressures without exhibiting shock symptoms.
Practical Implications for Trauma Care
In clinical practice, especially in trauma care, these insights necessitate a broader approach to patient assessment and management. Professor Harris emphasized the need to consider the mechanism of injury and other contextual factors in addition to traditional clinical signs. Understanding the energy transfer involved in an incident, such as a motorbike accident, can provide crucial information about potential internal injuries and blood loss.
Professor Harris advocates for a comprehensive approach that includes assessing the mechanism of injury, physiological responses, and potential complications. This method helps in making informed decisions about subsequent actions, such as whether a patient should go for a CT scan or directly to surgery. One key concept he highlighted was hemostatic resuscitation. In cases of major trauma, the priority may not always be to restore normal organ perfusion immediately but to maintain sufficient blood volume and prevent further deterioration. This approach often involves the use of blood products like fresh frozen plasma (FFP) and packed red cells, guided by a massive transfusion protocol.
Challenges and Considerations in Clinical Practice
Professor Harris also discussed the challenges of strictly adhering to guidelines. While guidelines provide valuable frameworks, they may not always apply perfectly to individual patient scenarios. The Advanced Trauma Life Support (ATLS) classification of shock into stages based on blood loss and physiological parameters often does not reflect real-world patient presentations. Factors such as medications, past medical history, pain, and anxiety can significantly alter a patient's physiological response to trauma.
This discrepancy underscores the importance of clinical judgment and experience in trauma care. Professor Harris emphasized that guidelines should be seen as tools to aid decision-making rather than rigid rules. Medical professionals must adapt these guidelines to the specific circumstances of each patient, taking into account their age, comorbidities, and overall clinical picture.
The Art and Science of Medicine
The conversation concluded with a reflection on the balance between the art and science of medicine. While evidence-based guidelines are essential, the true skill lies in applying these principles to individual patients. This requires a deep understanding of human physiology, extensive clinical experience, and the ability to think critically in high-pressure situations.
Professor Harris stressed the importance of continuous learning and professional development in mastering the complexities of trauma care. The more we learn about shock and trauma, the more we understand that simplistic models are insufficient. A holistic approach, considering the entire patient and their context, is crucial for effective care.
Key Takeaways
- Redefining Shock: Shock should be viewed as inadequate oxygen delivery rather than just low blood pressure.
- Cardiac Output and Oxygen Delivery: These are critical components of assessing shock, yet challenging to measure in real-time.
- Beyond Blood Pressure: Clinicians must consider the whole patient, including the mechanism of injury and physiological responses, rather than relying solely on blood pressure.
- Hemostatic Resuscitation: In major trauma, the focus may shift to maintaining blood volume and managing coagulopathy.
- Guidelines as Aids: While guidelines are useful, they should be adapted based on clinical judgment and the specific patient scenario.
- The Art of Medicine: The practice of medicine involves applying scientific knowledge with a nuanced understanding of each unique clinical situation.
Professor Tim Harris's insights challenge traditional approaches to shock and highlight the importance of a comprehensive, patient-centered approach in trauma care. This nuanced understanding of shock and trauma management is essential for improving patient outcomes and advancing the field of emergency medicine.

Wednesday Jan 14, 2015
Ep 34 - Intro to EM: Problems in Early Pregnancy
Wednesday Jan 14, 2015
Wednesday Jan 14, 2015
Managing Early Pregnancy Problems in the Emergency Department
Welcome to the St. Emelene's induction podcast. I'm Iain Beardsell, and I'm Natalie May. Today, we're discussing the management of early pregnancy problems in female patients presenting to the emergency department (ED). Some of you may rarely encounter these cases, while others may see them frequently. This podcast aims to provide a detailed guide on how to manage these patients effectively, optimizing our approach for better patient outcomes.
Understanding Early Pregnancy Problems
Early pregnancy problems can range from minor concerns to life-threatening emergencies. As emergency physicians, our primary goal is to identify and manage the worst-case scenarios promptly. In this post, we'll cover the following topics:
- Worst-case scenarios and initial steps
- History and physical examination
- Risk factors for ectopic pregnancy
- Diagnostic testing: urine vs. serum HCG
- Per vaginal (PV) examination: when to perform
- Management of threatened miscarriage
- Patient communication and support
Worst-case Scenarios and Initial Steps
In emergency medicine, we often think about the worst-case scenarios first. For early pregnancy problems, the most critical concern is an ectopic pregnancy. Ectopic pregnancies occur in about 1 in 100 pregnancies in the UK and can be life-threatening if not identified and treated promptly.
Initial Steps
When a young female patient presents with lower abdominal pain or spotting and is potentially pregnant, our first steps should include:
- Confirming pregnancy status: Use a urine pregnancy test initially.
- Assessing vital signs: Look for signs of hemodynamic instability, such as hypotension or tachycardia, which could indicate a ruptured ectopic pregnancy.
- Taking a detailed history: Understand the patient's symptoms, last menstrual period, and any previous gynecological issues.
History and Physical Examination
A thorough history and physical examination are crucial in managing early pregnancy problems. Here's what you need to focus on:
History
- Last Menstrual Period (LMP): Helps estimate the gestational age.
- Symptoms: Type and location of pain, nature of bleeding, and presence of other symptoms like dizziness or shoulder pain.
- Previous Pregnancies: Gravida (number of pregnancies) and Para (number of completed pregnancies).
- Risk Factors: Previous ectopic pregnancy, pelvic inflammatory disease, and any surgeries or procedures involving the reproductive organs.
Physical Examination
- Abdominal Examination: Look for tenderness, guarding, or rebound tenderness.
- Vital Signs: Monitor for signs of shock or hemodynamic instability.
- Pelvic Examination: In specific cases, to assess for cervical motion tenderness, adnexal tenderness, or masses.
Risk Factors for Ectopic Pregnancy
Understanding the risk factors for ectopic pregnancy can help identify patients who need urgent evaluation. Risk factors include:
- History of pelvic inflammatory disease (PID)
- Previous pelvic or abdominal surgery
- Use of intrauterine devices (IUDs)
- Previous ectopic pregnancy
- Assisted reproductive techniques like IVF
- Anatomical abnormalities of the fallopian tubes or uterus
- Endometriosis
- Use of the progesterone-only pill
Diagnostic Testing: Urine vs. Serum HCG
Determining the pregnancy status and ruling out ectopic pregnancy requires accurate diagnostic testing. Here's a comparison between urine and serum HCG tests:
Urine HCG Test
- Sensitivity: About 96%, particularly when HCG levels are above 100.
- Specificity: High, meaning a positive result is reliable.
- Limitations: May give false negatives if HCG levels are very low, as seen in some ectopic pregnancies.
Serum HCG Test
- Sensitivity and Specificity: Both close to 100%, making it the preferred test for confirming pregnancy and assessing HCG levels.
- Usage: Particularly useful when urine tests are negative but clinical suspicion remains high.
When to Perform a Per Vaginal (PV) Examination
The necessity of PV examinations in the ED can be debated. However, they are essential in specific situations:
- Retained Foreign Bodies: Such as condoms or tampons.
- Significant Vaginal Bleeding: Particularly in cases of suspected cervical shock due to retained products of conception.
For other scenarios, PV examinations are best left to gynecology specialists who have the expertise and appropriate setting to perform these exams with the required sensitivity and specificity.
Management of Threatened Miscarriage
A threatened miscarriage involves vaginal bleeding in a pregnancy less than 24 weeks, with a closed cervical os. It is a common issue that can cause significant anxiety for patients. Here's how to manage these cases:
Terminology
- Threatened Miscarriage: Vaginal bleeding with a closed cervical os.
- Inevitable Miscarriage: Open cervical os, indicating that miscarriage is likely to proceed.
- Complete Miscarriage: All products of conception have passed.
- Incomplete Miscarriage: Some products remain, requiring further management.
Approach
- Assess Bleeding: Light bleeding can often be managed on an outpatient basis. Heavy bleeding requires immediate gynecological consultation.
- Provide Reassurance: Explain that early pregnancy bleeding is common and not necessarily indicative of a miscarriage.
- Pain Management: Offer analgesia, such as paracetamol or cocodamol, to manage discomfort.
- Follow-up: Arrange for follow-up with an early pregnancy assessment unit (EPAU) within 48 hours.
Patient Communication and Support
Dealing with early pregnancy problems can be distressing for patients. Effective communication and support are crucial.
Tips for Communication
- Be Empathetic: Understand that this might be a significant and emotionally charged situation for the patient.
- Explain Clearly: Provide information about what is happening and what the next steps are.
- Avoid Definitive Statements: Unless certain, avoid saying that the patient has definitely miscarried.
- Offer Reassurance: Reiterate that early pregnancy complications are common and often not due to anything the patient did wrong.
Psychological Support
- Acknowledge Emotions: Recognize the patient's feelings and provide support.
- Encourage Support Systems: Suggest involving family or friends for emotional support.
- Professional Help: Refer to counseling services if needed.
Conclusion
Managing early pregnancy problems in the ED requires a systematic approach, starting with identifying worst-case scenarios and performing appropriate diagnostic tests. Understanding the risk factors for ectopic pregnancy and knowing when to perform a PV examination are crucial. Providing compassionate care and clear communication can help support patients through what can be a distressing time.
By optimizing our approach, we can ensure better outcomes for our patients and provide the best possible care in these challenging situations. Always consult senior colleagues when in doubt and follow local guidelines to ensure consistency and quality of care.
Tuesday Jan 06, 2015
Ep 33 - Impact Brain Apnoea with Gareth Davies from London HEMS (LTC 2014)
Tuesday Jan 06, 2015
Tuesday Jan 06, 2015
Understanding Impact Brain Apnea: A Revolutionary Insight into Trauma Care
Today, we delve into a fascinating and crucial topic in trauma care: impact brain apnoea. We recently had the privilege of attending the London Trauma Conference and caught up with Dr. Gareth Davis, a leading figure in trauma care and pre-hospital emergency medicine in the UK. Dr. Davis shared his insights into impact brain apnoea, a phenomenon that, while not widely recognized, has significant implications for patient outcomes.
The Unseen Danger: What is Impact Brain Apnoea?
Impact brain apnoea refers to a sudden cessation of breathing due to a blow to the head. This phenomenon, although not commonly discussed, has been a subject of intrigue for trauma professionals for many years. Dr. Davis explained that this condition occurs when an impact to the brain stem interrupts normal breathing, potentially leading to severe consequences if not promptly addressed.
This condition's significance lies in its subtlety and the challenges it poses in pre-hospital care. Many trauma incidents involve high-impact forces, such as car accidents, where a patient may suffer head injuries. Understanding the mechanics behind impact brain apnea can be the key to differentiating between minor and severe trauma cases, potentially saving lives.
The Historical Context and Research Challenges
The concept of impact brain apnoea isn't new, but it has been challenging to prove and widely accept due to a lack of concrete evidence. Gareth emphasized that the inconsistency in patient outcomes—where one individual might suffer severe consequences while another escapes with minor injuries—sparked curiosity among trauma specialists. Over time, through a combination of clinical observations and literature reviews, the medical community has started to piece together a more comprehensive understanding of this condition.
A significant barrier in researching impact brain apnoea is the timing of medical intervention. Most pre-hospital care teams arrive at the scene minutes after an incident, often too late to observe the initial apnea phase. This delay makes it challenging to gather real-time data, leaving a gap in understanding the immediate physiological responses post-trauma.
Physiological Mechanisms: The Dual Threat
Dr. Davis highlighted two critical physiological responses following a head injury that contributes to the complexity of treating impact brain apnea: the immediate cessation of breathing and a subsequent catecholamine surge.
-
Apnea and Hypoxia: The primary response is an apnea caused by the impact on the medulla oblongata, the brain's breathing control centre. This apnea leads to hypoxia (low oxygen levels) and hypercarbia (increased carbon dioxide levels), which can quickly deteriorate the patient's condition.
-
Catecholamine Surge: Following the initial apnea, the body releases a significant amount of catecholamines—hormones like adrenaline—that flood the system. This response, while a natural reaction to stress, can be detrimental, especially when the heart is already struggling due to hypoxia. The combination of these factors can lead to traumatic cardiac arrest, a situation where the heart fails due to trauma-induced physiological stress rather than direct injury.
Understanding these mechanisms is crucial for emergency responders. Recognizing the signs of impact brain apnea and addressing them promptly can be the difference between life and death.
The Clinical Conundrum: Diagnosing and Treating Impact Brain Apnea
One of the most challenging aspects of dealing with impact brain apnea is the clinical presentation. Patients may not exhibit obvious signs of severe trauma, such as external bleeding or visible injuries, making it difficult to diagnose based solely on physical examination. Gareth discussed the importance of thorough history-taking and observing indirect signs—akin to observing the "echo" of a particle, like in the Higgs boson analogy.
The lack of direct evidence means clinicians often rely on a combination of observational data, patient history, and situational awareness. For example, if a patient presents with persistent hypotension without a clear source of bleeding, clinicians might consider central shock—a term used to describe shock due to central nervous system dysfunction rather than volume loss.
The Role of Public Education and Pre-Hospital Care
Gareth emphasized the crucial role of public education and pre-hospital care in managing impact brain apnoea. The public's ability to provide immediate aid, such as opening an airway and administering ventilatory support, can significantly affect outcomes. He pointed out that while there is a global trend to focus on chest compressions in cases of cardiac arrest, for patients with traumatic injuries, addressing airway and breathing is paramount.
In London, initiatives like the GoodSAM app are helping bridge the gap by connecting trained responders with emergencies in real-time. This app allows people with medical training to provide critical first aid before professional services arrive, potentially mitigating the effects of impact brain apnea by ensuring the patient's airway is open and they are breathing adequately.
Navigating the Future: Research and Education
The conversation with Dr. Davis also highlighted the future directions for research and education. The medical community needs to invest more in understanding and validating the concept of impact brain apnea. This investment includes funding for clinical studies and fostering an environment where healthcare professionals can share their observations and experiences.
Podcasts, blogs, and medical conferences are valuable platforms for disseminating information about new medical phenomena like impact brain apnea. Dr. Davis encouraged medical professionals to remain curious, continue their education, and be open to emerging concepts that may not yet have robust evidence but have practical significance in clinical settings.
Key Takeaways and Clinical Pearls
-
Recognition and Belief: Clinicians need to recognize and believe in the concept of impact brain apnea. Even if direct evidence is scarce, understanding the physiological mechanisms and potential clinical presentations can guide effective treatment.
-
Focus on Airway and Breathing: In cases of traumatic injury, especially with suspected head trauma, the immediate focus should be on ensuring the airway is clear and the patient is breathing. This intervention can prevent the cascade of negative physiological responses that lead to traumatic cardiac arrest.
-
Role of Bystanders and First Responders: Public education and the involvement of trained responders are critical. Tools like the GoodSAM app can play a significant role in ensuring timely intervention.
-
Continuous Learning and Adaptation: The medical field must remain adaptive, incorporating new research findings and adjusting treatment protocols as more is understood about conditions like impact brain apnea.
Conclusion
Impact brain apnoea is a critical yet under-recognized phenomenon in trauma care. Through continued research, education, and public awareness, we can improve patient outcomes and provide better care in pre-hospital and clinical settings.

Thursday Dec 11, 2014
Ep 31 - London Trauma Conference: Day three round up.
Thursday Dec 11, 2014
Thursday Dec 11, 2014
Key Insights from the London Trauma Conference: Training, Innovation, and Clinical Governance in Emergency Medicine
Welcome to the St. Emlyn’s podcast summary of the London Trauma Conference. Over the past few days, experts in emergency medicine and pre-hospital care have shared valuable insights into the latest developments in our field. This blog post covers the highlights, focusing on effective training strategies, innovative practices, and crucial discussions on clinical governance.
Quality Education in Pre-Hospital Care by Cliff Reid
Cliff Reid’s session on delivering quality education in pre-hospital care was a standout. He emphasized that training for performance goes beyond knowledge acquisition. While understanding SOPs and the flip classroom approach are important, practical application is crucial.
Key Training Techniques:
- Stress Exposure Training: Regularly exposing doctors to high-pressure situations to build resilience.
- Perturbation: Introducing distractions during simulations to test team stability, such as simulating patient vomiting or monitor failures during an RSI procedure.
- Cross-Training: Ensuring paramedics and doctors train together and are evaluated as a team.
Cliff's insights highlight the necessity of training cohesive units to prepare effectively for real-world scenarios.
Learning from Failures in Modern Forensic Pathology
Professor Guy Ratti discussed modern forensic pathology, focusing on how clinical techniques are applied post-mortem to determine causes of death. The use of CT scans, angiography, and point-of-care toxicology testing has revolutionized post-mortem investigations, providing quicker and more detailed insights.
Learning Points:
- Application of Clinical Techniques Post-Mortem: Using CT scans and angiography to identify trauma causes.
- Point-of-Care Toxicology Testing: Rapid results within 45 minutes that can guide future clinical decisions.
For pre-hospital providers, understanding these techniques helps in learning from patients who couldn’t be saved, improving future care strategies.
Clinical Governance: Striking the Right Balance
Clinical governance was a key theme, with discussions on its importance and implementation. Effective governance structures are essential for ensuring consistent, high-quality care.
Governance Highlights:
- Structured and Regular Feedback: Creating environments where teams feel comfortable receiving and acting on feedback.
- Balancing SOP Adherence and Flexibility: Recognizing situations where deviation from SOPs is necessary for patient care.
The consensus was that governance must be tight enough to maintain standards but flexible enough to accommodate individual patient care nuances.
Transporting and Transferring Difficult Patients
A session dedicated to transporting and transferring difficult patients in the HEMS context provided practical advice and highlighted innovative approaches from international contingents.
Patient Categories:
- Psychiatric Patients: Safe sedation with ketamine for acutely psychotic patients.
- Bariatric Patients: Innovative positioning techniques, such as using a vac mat for intubation.
- Infectious Disease Patients: Protocols for safely managing and transporting patients with infectious diseases.
These insights are valuable for those working in diverse and challenging environments, ensuring patient safety and effective care during transfers.
Afternoon Sessions: EMS Disasters and Quick Hits
The afternoon sessions covered a range of topics, from emotional accounts of EMS disasters to rapid-fire discussions on current practices.
EMS Disasters:
- Case Studies from Norway and Glasgow: Brave speakers shared their experiences, offering lessons on safety and crisis management.
Quick Hits:
- Cervical Collars Debate: Discussing the efficacy and necessity of cervical collars, with evidence suggesting limited benefit but continued standard use.
- Pre-Hospital Blood Testing: Advocating for the feasibility and benefits of conducting blood tests in the pre-hospital environment.
These sessions underscored the importance of staying updated with current debates and practices, continuously evaluating and improving methods.
Innovation in Medical Technology: The GoodSAM App
Mark Wilson’s presentation on the GoodSAM app showcased how technology can revolutionize emergency response. The app alerts trained responders to nearby cardiac arrests, potentially saving lives by reducing response times.
Key Features:
- Free to Download: Available on both the App Store and Google Play.
- Community-Based: Encourages both medical and non-medical individuals to participate.
This app exemplifies how digital innovation can enhance traditional emergency response mechanisms, making it a must-have tool for responders and a valuable resource for the community.
Apnoeic Oxygenation During RSI
Cliff Reid returned to discuss apnoeic oxygenation during RSI, a technique that can extend the safe apnea period and reduce the risk of desaturation during intubation.
Practical Tips:
- Use of Nasal Oxygenation: Attach nasal specs to the patient in addition to mask ventilation.
- Simulation and Practice: Regular training to integrate this practice seamlessly into procedures.
This straightforward yet effective technique can significantly improve patient outcomes during RSI, both in pre-hospital and hospital settings.
Reflections and Future Directions
The London Trauma Conference provided a wealth of knowledge, practical advice, and innovative ideas for improving emergency medicine and pre-hospital care. From advanced training techniques to embracing new technologies and refining clinical governance, the insights shared by experts like Cliff Reid, Guy Ratti, and Mark Wilson are invaluable.
Key Takeaways:
- Emphasize team-based training and resilience-building techniques.
- Leverage modern forensic methods to learn from patient outcomes.
- Maintain structured yet flexible clinical governance.
- Implement innovative practices for transporting difficult patients.
- Stay updated with current debates and emerging technologies.
We hope these insights inspire you to reflect on your practices and consider how you can integrate these ideas into your work. Keep pushing the boundaries of emergency medicine, and stay tuned for more updates and interviews from the St. Emlyn’s team.
Keywords: London Trauma Conference, emergency medicine, pre-hospital care, clinical governance, forensic pathology, Cliff Reid, GoodSAM app, apnoeic oxygenation, cervical collars, blood testing, trauma training, EMS disasters, St. Emlyn’s.

Saturday Nov 29, 2014
Ep 27 - Intro to EM: The patient with chest pain
Saturday Nov 29, 2014
Saturday Nov 29, 2014
Top Five Diagnoses to Rule Out in Patients with Chest Pain
In emergency medicine, our primary objective is to rule out life-threatening conditions first. This principle guides our approach to patients with chest pain. Here are the top five diagnoses to consider:
- Acute Coronary Syndrome (ACS)
- Pulmonary Embolism (PE)
- Pneumothorax
- Pneumonia
- Aortic Dissection
These conditions can have overlapping symptoms but differ significantly in their management and prognosis. Let’s explore these further.
Acute Coronary Syndrome (ACS)
When a patient presents with chest pain, ACS is often the first concern. Key symptoms include central crushing chest pain, which may radiate to the arm or neck. While classic presentations are familiar to most, not all patients exhibit textbook symptoms. Factors like age, gender, and comorbidities can alter the clinical picture.
Initial Assessment and ECG Interpretation
Every patient with chest pain should receive an ECG as part of the initial workup. Interpreting ECGs requires a high level of expertise, as subtle changes can indicate significant pathology. In our department, only senior emergency physicians are tasked with reading initial ECGs to minimize the risk of missing critical findings. It's important to assess each ECG independently, even if previous records are available, as baseline abnormalities can obscure new, acute changes.
Troponin Testing
For patients where myocardial ischemia is suspected, a troponin test, particularly high-sensitivity troponin, is essential. This biomarker helps identify myocardial injury, even in cases where the ECG does not show definitive changes. Given the serious implications of missing an ACS diagnosis, a low threshold for testing is prudent. Approximately 10% of patients with a normal ECG may still have significant disease, highlighting the importance of comprehensive evaluation.
Pulmonary Embolism (PE)
Pulmonary embolism is another critical condition to consider, especially in patients presenting with pleuritic chest pain, shortness of breath, or risk factors such as recent immobilization, malignancy, or surgery. The clinical presentation of PE can vary, complicating diagnosis.
Clinical Decision Tools
The Wells score and PERC (Pulmonary Embolism Rule-out Criteria) are valuable tools in assessing the likelihood of PE. For low-risk patients, D-dimer testing can be used to rule out the condition, reducing the need for further imaging. However, for patients deemed at higher risk, CT pulmonary angiography (CTPA) is the gold standard for diagnosis. The decision to pursue imaging should be guided by clinical judgment and, where necessary, discussed with senior colleagues to avoid unnecessary radiation exposure and follow-up testing.
Pneumothorax
Pneumothorax should be considered in both young, otherwise healthy individuals and older patients with underlying lung disease. The hallmark symptom is sudden onset pleuritic chest pain, often accompanied by shortness of breath.
Diagnostic Approach
A chest x-ray is typically sufficient to diagnose pneumothorax. Given the low radiation dose and high diagnostic yield, x-rays should be performed for most patients with suspected pneumothorax. The imaging will not only confirm the presence of air in the pleural space but also help assess the severity and guide management decisions.
Pneumonia
Pneumonia is a common cause of chest pain, often accompanied by fever, cough, and sputum production. It is more common in patients with a history of respiratory disease or immunosuppression.
Identifying Pneumonia
A chest x-ray remains the cornerstone of pneumonia diagnosis. Clinical symptoms, such as productive cough and fever, along with imaging findings of consolidation, help differentiate pneumonia from other causes of chest pain. While not immediately life-threatening in most cases, timely recognition and treatment are crucial to prevent complications.
Aortic Dissection
Aortic dissection is a less common but highly dangerous cause of chest pain. Classic symptoms include severe, tearing pain radiating to the back. It is critical to maintain a high index of suspicion for aortic dissection, especially in patients with risk factors such as hypertension, connective tissue disorders, or a family history of the condition.
Confirmatory Testing
The definitive diagnostic test for aortic dissection is a CTA aortogram. While a chest x-ray can sometimes reveal mediastinal widening, it is not sufficiently sensitive to rule out dissection. Early consultation with cardiothoracic surgery and rapid imaging are key to managing suspected cases.
Communicating with Patients
Once life-threatening causes have been ruled out, patients often seek answers about their symptoms. When the etiology remains unclear, it’s important to communicate transparently with the patient. Possible benign causes include musculoskeletal pain or gastroesophageal reflux disease (GERD). While it’s reassuring to exclude serious conditions, acknowledging the limitations of our diagnostic tools and advising patients to return if symptoms change is crucial.
Patient Reassurance and Follow-up
Patients should be advised to follow up with their primary care physician for further evaluation and management of non-urgent conditions. Clear communication, including documenting your diagnostic reasoning and plan, is vital for medico-legal protection and patient safety.
Conclusion: Mastering Chest Pain in the ED
Chest pain remains a complex and multifaceted challenge in the emergency department. The ability to swiftly differentiate between benign and life-threatening causes is a critical skill for emergency physicians. Our approach should be guided by a thorough history, physical examination, and appropriate use of diagnostic tools. Remember, the primary goal is to exclude serious conditions, ensuring patient safety while avoiding unnecessary investigations.
As you continue your journey in emergency medicine, refine your skills in evaluating chest pain. Be diligent in your assessments, stay updated with the latest guidelines, and always communicate clearly with your patients and colleagues. This comprehensive approach will not only improve patient outcomes but also enhance your clinical practice.
Read the blog post here

Wednesday Nov 12, 2014
Ep 24 - Getting started in Emergency Medicine Research
Wednesday Nov 12, 2014
Wednesday Nov 12, 2014
The Challenge and Value of Research in Emergency Medicine: at DGINA 2014
Rick Body's talk from DGINA on the need for research in EM.
Check out the associated blog post at http://stemlynsblog.org

Friday Oct 31, 2014
Ep 23 - Smacc Chicago update
Friday Oct 31, 2014
Friday Oct 31, 2014
Exciting Updates from St. Emlyn's: Highlights, Conferences, and Upcoming Events
Welcome to the St. Emlyn's Podcast Recap
Greetings, St. Emlyn's community! We are delighted to bring you the latest updates and highlights from our podcast and blogosphere. Let's dive into our recent achievements, exciting conferences, and what's on the horizon for our team.
Highlights from the Past Few Months
The past few months have been phenomenal for St. Emlyn's. Our blog has seen a surge in readership, and we’ve received fantastic feedback on various posts and podcast episodes. One standout topic has been the work on high-sensitive troponin, thanks to Rick's invaluable insights. Even those of us working with troponin in our department found new learnings through the podcast.
Another high point was Natalie May's episode on button battery ingestion in children. This critical topic resonated with many of our listeners and highlighted the dangers and necessary precautions surrounding this issue. Additionally, having Alan Grayson critique NICE guidelines on heart failure provided us with fresh perspectives and sparked meaningful discussions within our virtual hospital.
Conferences and Collaborations
Our team has been active on the conference circuit, sharing knowledge and gaining new insights. The European Society of Emergency Medicine (EUSEM) conference in Amsterdam was a significant event, offering a plethora of information and networking opportunities. Natalie is even planning to produce a book and podcast to summarize the key takeaways from the conference.
Down in Exeter, the Chem conference exceeded expectations. Adam Ruben’s podcast recap provided a comprehensive overview of the event, and we had the pleasure of paddleboarding with Cliff Reed, adding a bit of fun to the professional gathering.
The Evolution of Emergency Medical Conferences
Emergency medical conferences have evolved remarkably over the past decade. The variety and depth of content offered now are impressive. Our team is already gearing up for the Chem conference in Manchester next September, and the recently released program for SMACC Chicago has everyone buzzing with excitement.
SMACC Chicago: A Preview
The SMACC conferences are renowned for their exceptional quality and dynamic content, and SMACC Chicago is no exception. The program is packed with sessions from leading experts in emergency medicine, making it challenging to choose which talks to attend. Simon Carley will be presenting alongside luminaries like Scott Weingart, Pat Cross-Kerry, Ashley Shree, and Stephen Mayer, promising a wealth of knowledge and inspiration.
The release of the SMACC Chicago program has us eagerly anticipating the event. With five streams of information, choosing which sessions to attend will be a delightful dilemma. Highlights include sessions with Karim Brohee, Paul Marik, Rick Body, and Louise Cullen. Simon is excited to be part of such an esteemed lineup, despite the stiff competition.
Workshops and Debates
Before the main conference kicks off, a series of workshops will provide hands-on learning experiences. Simon will join Scott from the Medical Evidence Blog, Ken Milne from SGEM, Rob McSweeney, Rick Body, and David Newman from Smart EM to discuss evidence-based emergency medicine. It’s an incredible opportunity to learn from and with the best in the field.
One of the anticipated sessions is the SMACC Chicago forum on Thursday afternoon, featuring debates and discussions on topics that matter deeply to the emergency medicine community. The session titled “Seeking the Truth” promises to be a highlight, with speakers like Paul Young and Simon Finfer discussing randomized controlled trials (RCTs).
Networking and Building Connections
Conferences like SMACC are not just about attending sessions—they’re about building connections and forming lasting relationships with peers and mentors. Meeting the greats of emergency medicine, such as Dave Newman, and discussing both cutting-edge topics and the human side of medicine, makes these conferences invaluable.
The Value of Investing in Education
While attending conferences can be a significant financial investment, the benefits far outweigh the costs. The opportunity to learn from leading experts, network with peers, and stay updated on the latest advancements in emergency medicine makes these events a crucial part of professional development. For those considering attending SMACC Chicago, registration opens on the 5th of November. Early registration for trainees, nurses, and paramedics offers a more affordable way to join this transformative event.
What's Next for St. Emlyn's?
Looking ahead, we have a robust lineup of podcasts and blog posts planned. Our induction series continues to provide valuable insights for new doctors entering emergency medicine departments across the UK. We’re also exploring topics like Gestalt and clinical thinking to deepen our understanding and improve patient care.
Join the Conversation: Get Involved with St. Emlyn's
We want to hear from you! Your feedback helps us tailor our content to meet your needs. Connect with us on Facebook, rate us on iTunes, and share your thoughts and ideas. We’re always looking for guest writers to contribute to our blog. If you have a topic you’re passionate about, reach out to us and join the St. Emlyn's community.
A Special Thanks
A special thanks to Sarah Payne for her timely articles on Ebola, which have been incredibly well-received. Her contributions have enriched our blog, providing vital information and sparking meaningful discussions.
Enjoy Your Emergency Medicine Journey
At St. Emlyn's, our mission is to make your emergency medicine journey more enjoyable and fulfilling. We’re committed to enhancing your professional development and patient care through engaging content and insightful discussions.
Stay tuned for more podcasts, blog posts, and exciting updates. Don’t forget to register for SMACC Chicago and join us for an unforgettable experience.
Thank you for being part of the St. Emlyn's community. Enjoy your emergency medicine journey, have fun, and go forth and heal the sick. We’ll be back soon with more exciting content and updates.

Friday Oct 31, 2014
Ep 22 - Button Battery ingestion in children
Friday Oct 31, 2014
Friday Oct 31, 2014
The Danger of Button Batteries: Essential Information for Emergency Physicians
Introduction
Hello and welcome to the St Emlyn's blog. I'm Simon Carley, and alongside me is Natalie May. This post addresses a frequent and potentially serious issue in emergency departments: the ingestion of button batteries. With Halloween and Christmas approaching, these small but hazardous objects become more prevalent in households with small children. Here, we provide critical insights for emergency physicians on identifying, managing, and preventing complications related to button battery ingestion.
Understanding Button Battery Ingestion
Button batteries, or disc batteries, are small, round batteries found in devices like watches, musical badges, and holiday decorations. Their size and shiny appearance make them attractive to children, who may ingest them or insert them into their noses or ears. While they appear harmless, button batteries can cause significant harm if they become lodged in mucosal surfaces.
The Risks of Button Battery Ingestion
When a button battery becomes wedged against a mucosal surface, it generates a small electrical current. This current can cause chemical burns and tissue damage within as little as two hours. If not promptly removed, the battery can lead to severe complications, including death.
Common Scenarios and Symptoms
Children often ingest various objects, but button batteries pose a unique risk due to their electrical properties. Here are common scenarios and symptoms to watch for:
- Ingestion: Symptoms range from mild (drooling, difficulty swallowing) to severe (vomiting, abdominal pain, gastrointestinal bleeding).
- Nasal Insertion: Batteries in the nose can cause nasal discharge, pain, and significant tissue damage if unnoticed.
- Ear Insertion: Batteries in the ear can lead to pain, discharge, and hearing loss if not promptly addressed.
Radiological Identification
Button batteries are radiopaque, making them visible on X-rays. They can be distinguished from coins by their characteristic double shoulder appearance. This feature is crucial for accurate diagnosis and timely intervention.
Management Strategies
Immediate Steps for Suspected Ingestion
- High Index of Suspicion: Be vigilant for signs of button battery ingestion, especially if parents report missing batteries from devices.
- Radiological Examination: Perform an X-ray to locate the battery and determine its position.
Removal from Ears and Noses
- ENT Referral: Button batteries in the nose or ears should be removed promptly by an ear, nose, and throat specialist. These areas are less moist than the esophagus but can still suffer chemical burns and tissue damage.
Esophageal Ingestion
- Surgical Emergency: Batteries lodged in the esophagus must be removed immediately. This task is typically handled by general surgeons or gastroenterologists. Delaying removal can lead to severe complications, including perforation, erosion into blood vessels, and catastrophic bleeding.
Post-Removal Care and Follow-Up
Even after successful removal, children must be monitored for complications. Discharge instructions should include warning signs such as gastrointestinal bleeding, severe abdominal pain, vomiting, respiratory distress, and refusal to eat. Follow-up appointments and possibly additional X-rays are essential to ensure no further damage has occurred.
Prevention Tips for Parents
Educating parents about the dangers of button batteries is crucial. Here are some tips to share with them:
- Secure Storage: Keep button batteries out of reach of children.
- Device Safety: Ensure battery compartments in devices are secure and childproof.
- Immediate Action: If a battery is missing and a child shows symptoms of ingestion, seek medical attention immediately.
Case Studies and Real-Life Examples
Case 1: Nasal Insertion
A child was brought to the emergency department with a suspected nasal insertion of a button battery. Despite a thorough examination, no battery was visible. However, an X-ray revealed a large button battery lodged in the posterior nose. Prompt referral to ENT and removal prevented further complications.
Case 2: Esophageal Lodgment
A child swallowed a button battery that became lodged in the esophagus. The battery was removed within two hours, but the child was monitored closely for weeks due to the risk of delayed complications. Despite initial removal, the child developed severe symptoms days later, highlighting the importance of vigilant post-removal care.
Conclusion
Button batteries pose a significant risk to children, particularly during festive seasons when they are more prevalent in households. Emergency physicians must maintain a high index of suspicion, utilize radiological tools effectively, and act swiftly to manage cases of ingestion or insertion. Educating parents about the dangers and prevention strategies is equally important. Stay vigilant, stay informed, and ensure the safety of our youngest patients.
Additional Resources
For more information on button battery ingestion and other pediatric emergencies, visit the St Emlyn's blog. Follow us on Facebook and join our community of emergency medicine professionals dedicated to providing the best care for our patients.

Tuesday Oct 28, 2014
Ep 21 - Code for Cash and Credibility
Tuesday Oct 28, 2014
Tuesday Oct 28, 2014
The Crucial Role of Accurate Coding in Emergency Medicine: Insights from St Emlyns
Welcome to the St Emlyns blog! Today, we dive into a topic often overlooked but crucial to the functioning and financial health of emergency departments (ED): coding. This subject might not have the drama of resuscitations or surgical interventions, but it significantly impacts how we are perceived and funded. In this post, we explore how coding works in the context of emergency medicine in England, why it matters, and how we can improve our practices for better outcomes.
Understanding Coding in Emergency Departments
What is Coding?
In the simplest terms, coding is the process of translating medical activities into standardized codes that determine how much a hospital gets paid for the services provided. This is done through systems like the HRG-4 (Health-Related Grouping) codes, which classify the treatments and investigations performed on patients.
Why is Coding Important?
Accurate coding is essential because it directly affects the revenue of an emergency department. The details recorded in discharge summaries play a significant role in determining the funds a hospital receives. For instance, different procedures and investigations, like CT scans or blood tests, have specific codes that contribute to the total amount of money paid to the hospital.
The Financial Implications of Coding
Top Earning Codes in Emergency Medicine
The highest amount an ED can earn for a single patient episode is £237, applicable in cases involving resuscitation, thrombolysis, or laser eye surgery. However, if no tests or treatments are performed, the hospital only earns £58 for that patient. This stark difference underscores the importance of detailed and accurate coding.
Common Investigations and Their Codes
- MRI/CT Scans: High-value procedures that significantly boost the hospital's revenue.
- Ultrasound Scans: Similarly valued to MRI/CT scans, contributing substantial amounts to the hospital's income.
- Vital Signs Recording: Even basic procedures like recording vital signs can elevate the payment from the lowest tariff.
Challenges in Implementing Accurate Coding
Perception vs. Reality
Many healthcare professionals, including doctors and nurses, often view coding as an administrative burden rather than a critical part of patient care. This perception needs to change, as the quality of coding affects not only financial outcomes but also how the department's efficiency and effectiveness are perceived by external bodies like the CCG (Clinical Commissioning Groups).
The Role of IT Systems
Modern IT systems have made the coding process more streamlined, though they are not without their challenges. Integrating coding tasks into daily routines, such as through discharge summaries and GP letters, can help ensure that all activities are recorded accurately.
Improving Coding Practices
Education and Awareness
Educating staff about the importance of coding and its impact on both departmental funding and patient care is crucial. Junior doctors and new consultants should be made aware of how their input affects the overall picture.
Dedicated Coding Staff
Some hospitals have experimented with employing dedicated coding staff who review and correct coding entries, leading to significant increases in revenue. This approach can alleviate the burden on clinicians and ensure more consistent and accurate coding.
Streamlining Processes
Integrating coding into clinical workflows can make it less of a chore. For example, requesting an X-ray through the hospital's system should automatically record it in the patient's coding data. Such improvements can simplify the process and reduce the likelihood of missed entries.
The Impact of Coding on Departmental Perception
Meeting Standards and Avoiding Fines
In England, EDs are required to meet specific standards, such as the four-hour wait time target. Failing to meet these standards can result in fines, which further strain departmental resources. Accurate coding helps present a true picture of the department's workload and efficiency, potentially mitigating some of these financial penalties.
Communicating with Commissioners
Accurate coding ensures that commissioners have a clear understanding of the services provided by the ED. Misrepresentations can lead to misconceptions about the department's performance and the appropriateness of patient attendances, affecting future funding and policy decisions.
Case Study: VB11Z Code
The VB11Z code, which indicates that no investigations or treatments were performed, often misrepresents the actual work done in the ED. For example, patients admitted under the care of other specialists but using ED resources might be incorrectly coded, leading to a loss of revenue. By addressing such coding inaccuracies, departments can better reflect their true workload and resource needs.
Practical Tips for Better Coding
Record Everything
Ensure that all procedures, tests, and treatments are recorded, no matter how minor they might seem. This includes vital signs, which can elevate the payment bracket significantly.
Integrate Coding with Patient Care
Make coding part of the routine patient care process. For example, use discharge summaries to not only inform GPs but also to ensure all activities are coded.
Leverage Technology
Utilize the full capabilities of IT systems to automate and streamline coding tasks. This can reduce the manual burden and improve accuracy.
Continuous Training
Regularly update staff on coding practices and the importance of accurate data entry. This helps maintain awareness and reduces the risk of complacency.
Conclusion
While coding might not be the most glamorous aspect of emergency medicine, it is undeniably one of the most crucial. Accurate coding not only ensures that departments are properly funded but also that they are accurately represented in terms of workload and efficiency. By integrating better coding practices into daily routines and educating staff on its importance, emergency departments can significantly improve their financial health and operational effectiveness.
For more detailed information, including specific codes and their values, visit our blog or contact us directly. Keep coding and keep improving patient care!

Tuesday Sep 23, 2014
Ep 18 - Victoria Brazil on great presentations with St.Emlyn's
Tuesday Sep 23, 2014
Tuesday Sep 23, 2014
Mastering the Art of Presentation: Insights from St. Emlyns and Victoria Brasile
Welcome to the St. Emlyns blog! I'm Iain Beardsell, and today, we're diving into a recent enlightening session with the rest of the St. Emlyns team—Simon, Nat, and Rick—alongside the exceptional educator, Victoria Brasile. Victoria recently visited the UK and shared invaluable tips on delivering excellent presentations to the emergency medical community in Manchester. For those familiar with Victoria’s engaging talks at SMACC, either in person or online, you're in for a treat as we explore the key points from this memorable evening.
The Power of a Great Presentation
Victoria Brasile's visit was a golden opportunity for the emergency medicine community. Her session focused on how to deliver impactful presentations—an essential skill for any healthcare professional. Here are the core messages she shared:
- Connect with Your Audience: Establishing a strong connection with your audience is fundamental.
- Look and Sound Great: Presentation is not just about content but also about delivery.
- Keep It Simple: Simplicity ensures clarity and retention.
These principles form the bedrock of an excellent presentation, whether addressing a large lecture hall, a small group, or even a single patient.
Connecting with the Audience
Victoria emphasized the importance of making a genuine connection with your audience. She believes that regardless of the audience size, the ability to connect on a personal level is crucial. Here’s how you can achieve this:
- Engage Interactively: Encourage audience participation by asking questions or incorporating interactive elements.
- Use Relatable Stories: Share anecdotes that resonate with the audience’s experiences.
- Maintain Eye Contact: Establishing eye contact can make your audience feel involved and valued.
During the Manchester session, Victoria practiced what she preached by fostering interaction and creating an inclusive environment. Her approach demonstrated how effective communication can transform a presentation into an engaging dialogue.
The Importance of Presentation
Victoria highlighted that looking and sounding great goes beyond mere aesthetics; it’s about being confident and authentic. Here are her top tips:
- Dress Appropriately: Your attire should be professional but comfortable, ensuring you feel confident.
- Voice Modulation: Vary your tone to maintain interest and emphasize key points.
- Body Language: Use purposeful gestures to reinforce your message and avoid distracting habits.
In Manchester, Victoria’s presentation was a masterclass in these techniques. Her confident demeanor, combined with dynamic voice modulation and engaging body language, kept the audience captivated.
Simplicity is Key
The third cornerstone of a great presentation is simplicity. Victoria advised that a clear and straightforward message is more likely to be remembered and appreciated. Here’s how to keep it simple:
- Focus on Key Points: Identify and emphasize the main takeaways.
- Avoid Jargon: Use language that is easily understandable, avoiding technical terms unless necessary.
- Visual Aids: Use slides and visuals that are clear and directly related to your points.
Victoria’s own presentations are a testament to this principle. She distilled complex information into easily digestible parts, ensuring her audience could follow along and retain the key messages.
Lessons from the St. Emlyns Team
Our team also shared their reflections and learnings from Victoria’s session:
Rick Boddie: Managing Nerves
Rick found the session particularly insightful for managing presentation nerves. He realized that controlling nerves is essential not only for the speaker but also for the audience’s comfort. Rick’s takeaway included:
- Preparation and Practice: Regular practice to build confidence.
- Breathing Techniques: Simple breathing exercises to calm nerves.
- Audience Empathy: Recognizing that the audience might be just as nervous.
Natalie May: Planning for Interaction
Natalie focused on incorporating audience interaction into her presentations. She plans to use:
- Social Media and Technology: Integrating modern tools to engage the audience.
- Structured Interactivity: Planning specific moments for audience participation.
- Pacing: Slowing down her speech to ensure clarity and engagement.
Simon Carly: First Impressions
Simon highlighted the importance of making a strong first impression. His key points included:
- Immediate Engagement: Captivating the audience right from the start.
- Preparation: Ensuring thorough preparation before stepping onto the stage.
- Action-Packed Opening: Starting with a memorable and impactful opening, akin to a Bond movie.
Enhancing Audience Interactivity
Victoria’s innovative approach to audience interaction was a standout feature of her session. She shared how dedicating a few minutes for the audience to interact amongst themselves can enhance the overall experience. This strategy not only breaks the ice but also makes the audience feel more connected and engaged. During her SMACC Gold talk, Victoria’s use of theatre—changing the stage setup and creating a visually intriguing environment—demonstrated how a bit of drama can capture and hold the audience’s attention.
Conclusion: The Three Pillars of a Great Presentation
Victoria Brasile’s session at Manchester reinforced the three pillars of a great presentation: connecting with the audience, looking and sounding great, and keeping it simple. These principles are not just theoretical; they are actionable strategies that any speaker can implement to enhance their presentations. The St. Emlyns team’s reflections further underscore the importance of preparation, interaction, and first impressions.
As we continue to learn and grow in our professional journeys, let’s keep these valuable lessons in mind. Whether you’re presenting at a conference, teaching a class, or communicating with patients, these insights will help you deliver your message more effectively and confidently.
Stay tuned for more insights and tips from the St. Emlyns team. We hope you enjoyed this deep dive into the art of presentation. Until next time, embrace your emergency medicine practice with enthusiasm and excellence!
For more resources and links to Victoria Brasile’s talks, visit our blog site. If you have any questions or thoughts to share, please leave a comment below. We’d love to hear from you!

Friday Sep 12, 2014
Ep 17 - Diffuse Axonal Injury with John Hell
Friday Sep 12, 2014
Friday Sep 12, 2014
Understanding and Managing Diffuse Axonal Injury in Neurointensive Care
Welcome to the St Emlyn’s blog. I’m Iain Beardsell, and today we delve into the complex and crucial topic of diffuse axonal injury (DAI) with insights from John Hell, a consultant in Neurointensive Care at the University Hospital of Southampton and former director of the Wessex Neuroscience’s Intensive Care Unit. With his extensive experience and co-authorship of the Neurointensive Care guidelines, John provides a comprehensive overview of DAI, its pathophysiology, management, and prognosis.
What is Diffuse Axonal Injury?
Diffuse axonal injury is a type of traumatic brain injury where the brain’s axons are sheared due to rapid acceleration or deceleration forces. This can occur in various scenarios, from minor to severe head injuries. The axons, which connect the grey matter (cell bodies) on the brain's surface to the white matter (nerve fibers) inside, are particularly susceptible to damage when subjected to such forces.
Pathophysiology of Diffuse Axonal Injury
The pathophysiology of DAI involves axonal shearing due to differing densities and connections between grey and white matter. When the brain moves at different rates within the skull during an injury, this shearing occurs. Initially, this stretching does not necessarily rupture the axons but causes them to swell and release mediators. These mediators lead to further axonal breakdown and secondary brain injury characterized by cerebral edema, increased intracranial pressure (ICP), and restricted diffusion of glucose and oxygen.
Clinical Presentation and Diagnosis
DAI can be challenging to diagnose initially, as early imaging might show minimal changes. However, small petechial hemorrhages at the grey-white matter interface can be indicative. These are more evident on MRI scans or repeat CT scans after 6 to 24 hours. Clinicians should be vigilant about mechanisms of injury, Glasgow Coma Scale (GCS) scores, and clinical presentation to suspect DAI.
Management Strategies in Neurointensive Care
The management of patients with DAI involves a multi-faceted approach focused on stabilizing and maintaining normal physiological parameters. Key steps include:
-
Initial Stabilization: Ensure normal blood pressure, oxygenation (PACO2 and PIO2), and venous drainage from the head by positioning the patient appropriately and avoiding obstructions like tight cervical collars.
-
Monitoring and Imaging: Initial imaging may show little, but repeat CT or MRI scans can reveal the extent of the injury. Placing an ICP monitor helps in maintaining adequate cerebral perfusion pressure (CPP) as ICP rises over 72 to 96 hours.
-
Intravenous Fluids: Use of normal saline is recommended due to its osmolality. Other fluids like Hartmann's, which are hypo-osmolar, can exacerbate cerebral edema by diluting plasma.
-
Anticoagulation Management: Reversal of anticoagulation and ensuring normal platelet function is crucial. Patients on anticoagulants should have these reversed immediately, and those on antiplatelet agents should receive platelet transfusions if still bleeding.
Prognosis and Outcomes
Prognosis in DAI is variable and often unpredictable based on initial presentation. While patients with poor GCS scores tend to do worse on average, individual outcomes can vary widely. Aggressive monitoring and management in neurointensive care units have shown that many patients can recover to independence and good quality of life, challenging the previous perception of uniformly poor outcomes.
Practical Insights for Emergency and Pre-Hospital Care
In emergency and pre-hospital settings, early interventions can significantly impact outcomes. Prioritizing normal physiological parameters, using appropriate induction agents, and ensuring timely referral to neurointensive care are essential steps. For instance, thiopental is recommended for induction in hemodynamically stable patients with isolated head injuries due to its efficacy in minimizing cerebral metabolic rate for oxygen (CMRO2). For unstable patients, ketamine remains a safe alternative despite old concerns about its use in head injuries.
Case Study and Practical Application
Consider a hypothetical case of a 45-year-old cyclist involved in a high-speed accident, resulting in severe head injury without intracranial bleed but with suspected DAI. The patient is intubated and ventilated by the pre-hospital team and transferred to a major trauma center. Initial CT shows minimal injury, but due to the mechanism and presentation, DAI is suspected.
In neurointensive care, management focuses on:
- Stabilization: Ensuring normal blood pressure, oxygenation, and venous drainage.
- Monitoring: Placing an ICP monitor and repeating imaging at 6, 12, or 24-hour intervals.
- Fluid Management: Using normal saline to maintain plasma osmolality.
- Anticoagulation Reversal: Reversing any anticoagulation and ensuring normal platelet function.
Over the next 72 to 96 hours, the patient’s condition is closely monitored, with adjustments made based on ICP readings and repeat imaging. The interdisciplinary team works together to minimize secondary brain injury and support recovery.
The Role of Education and Ongoing Research
Continuous education and staying updated with the latest guidelines and research are crucial for healthcare professionals managing traumatic brain injuries. The Neurointensive Care guidelines co-authored by John Hell and his team are a valuable resource available online, providing evidence-based practices for managing these complex cases.
Conclusion
Diffuse axonal injury remains a significant challenge in neurointensive care, requiring a comprehensive and multidisciplinary approach for optimal outcomes. Early recognition, aggressive management, and ongoing research are key to improving the prognosis for patients with DAI. By maintaining normal physiological parameters, utilizing appropriate fluids, and implementing timely interventions, healthcare professionals can make a substantial difference in the recovery and quality of life for these patients.
Thank you for joining us on the St Emlyn’s blog. We hope this detailed exploration of DAI provides valuable insights for your practice. Stay tuned for more discussions on critical topics in emergency and intensive care medicine.
Friday Aug 22, 2014
Friday Aug 22, 2014
Understanding Syncope: A Comprehensive Guide for Emergency Medicine
Introduction
Today, we are discussing syncope, a common yet complex condition involving a transient loss of consciousness due to a temporary reduction in blood flow to the brain. This comprehensive guide aims to provide insights into diagnosing and managing syncope in the emergency department.
The Challenge of Syncope Diagnosis
When patients present with collapse, it’s essential to differentiate between mechanical falls and syncope due to physiological reasons. The key to diagnosis lies in understanding whether the event was caused by a transient loss of consciousness or a mechanical fall. This distinction guides the diagnostic pathway and ensures the appropriate management of potential life-threatening conditions.
Physiology of Syncope
Syncope results from a temporary reduction in cerebral perfusion pressure, which can occur due to various physiological disruptions. Understanding the factors affecting cerebral perfusion, such as mean arterial pressure, cardiac output, and peripheral resistance, is crucial. Any significant deviation in these parameters can lead to syncope.
Cardiac Causes of Syncope
Rhythm Issues
Cardiac syncope often involves rhythm disturbances like bradycardia (abnormally slow heart rate) or tachycardia (abnormally fast heart rate). Bradycardia can reduce cardiac output, while tachycardia can decrease stroke volume. Identifying these rhythm issues is vital as they can be life-threatening.
Structural Issues
Structural heart diseases, such as aortic stenosis or hypertrophic cardiomyopathy, restrict blood flow, leading to syncope. Pulmonary embolism, although less common, can also cause syncope by obstructing pulmonary circulation.
Importance of ECG in Diagnosis
The electrocardiogram (ECG) is a critical tool for diagnosing cardiac causes of syncope. It helps identify arrhythmias, conduction abnormalities, and other cardiac issues. Continuous ECG monitoring, or Holter monitoring, can capture transient arrhythmias not seen on a standard ECG.
Neurological Causes of Syncope
Neurological conditions, such as seizures and transient ischemic attacks (TIAs), can present as syncope. Differentiating between these and true syncope is essential. Seizures often have specific signs like tongue biting, loss of bladder control, and post-ictal confusion. TIAs can cause temporary disruptions in blood flow to the brain, leading to syncope-like episodes.
Physiological Causes of Syncope
Vasovagal Syncope
Vasovagal syncope, triggered by stress, pain, or prolonged standing, involves a sudden drop in heart rate and blood pressure. It is a common and generally benign cause of syncope.
Orthostatic Hypotension
Orthostatic hypotension, a drop in blood pressure upon standing, can result from dehydration, medications, or autonomic dysfunction. It is a frequent cause of syncope, especially in elderly patients.
Diagnostic Approach
Patient History
A thorough patient history is crucial for identifying the cause of syncope. Key elements include the circumstances of the episode, prodromal symptoms, witness accounts, and medical history. This information helps distinguish between different causes of syncope.
Physical Examination
A comprehensive physical examination includes checking vital signs, cardiovascular examination, and neurological assessment. Identifying abnormalities during the physical exam can provide clues to the underlying cause of syncope.
Diagnostic Tests
- ECG: Identifies arrhythmias and conduction abnormalities.
- Holter Monitoring: Captures transient arrhythmias.
- Echocardiogram: Assesses structural heart diseases.
- Tilt-Table Test: Diagnoses vasovagal syncope or orthostatic hypotension.
- Blood Tests: Evaluate electrolyte levels, blood glucose, and cardiac biomarkers.
Management Strategies
Cardiac Syncope
Management of cardiac syncope focuses on stabilizing heart rhythm and function. Treatments may include pacemaker implantation for bradycardia, medications for tachycardia, and surgical interventions for structural heart diseases. Arrhythmias may require implantable cardioverter-defibrillators (ICDs).
Neurological Syncope
Managing neurological causes involves addressing the underlying condition. Antiepileptic medications control seizures, while immediate interventions restore blood flow in strokes or control bleeding. TIAs require medications and lifestyle changes to reduce recurrence risk.
Physiological Syncope
- Vasovagal Syncope: Management includes avoiding triggers, increasing fluid and salt intake, and using compression stockings. Severe cases may require medications.
- Orthostatic Hypotension: Gradual position changes, increased hydration, and reviewing medications. Medications like fludrocortisone may be necessary.
- Dehydration: Rehydration with oral or intravenous fluids.
- Medication Review: Adjusting or discontinuing medications contributing to syncope.
Safety Netting and Follow-Up
Safety netting ensures patients receive appropriate follow-up care and instructions. Key elements include providing clear discharge instructions, scheduling follow-up appointments, and educating patients about syncope causes and management.
Special Considerations
Reflex Anoxic Seizures
Reflex anoxic seizures, seen especially in children, involve shaking movements due to a drop in oxygenation. These can be misinterpreted as epileptic seizures but require different management.
Misdiagnosis Risks
Misdiagnosis of syncope as epilepsy or vice versa is common. Always consider both possibilities, especially when symptoms overlap.
Postural Hypotension and Specific Diagnoses
Postural hypotension requires careful evaluation. Special considerations include ruling out abdominal aortic aneurysm in older men and ectopic pregnancy in younger women.
Conclusion
Syncope is a multifaceted condition that demands careful evaluation and management in the emergency department. By understanding the underlying causes, utilizing appropriate diagnostic tools, and implementing effective management strategies, healthcare professionals can optimize patient outcomes and reduce the risk of recurrent episodes.
This guide aims to provide valuable insights into the diagnosis and management of syncope, helping healthcare providers deliver high-quality care. For further information, examples, and case studies, visit the St Emlyn's blog, where we continue to share knowledge and expertise in emergency medicine.
Remember, accurate diagnosis and timely intervention are key to managing syncope effectively. Stay vigilant, consult with senior colleagues when needed, and always prioritize patient safety.
Thank you for reading. If you have any questions or need further information, please get in touch. We look forward to continuing the conversation and improving patient care together.
Thursday Aug 07, 2014
Ep 15 - Understanding Troponin - Part 2
Thursday Aug 07, 2014
Thursday Aug 07, 2014
Understanding High Sensitivity Troponins: A Guide for Emergency Physicians
Welcome to the St. Emlyn's podcast. I'm Ian Beardsell and I'm Rick Bodden. This is part two of our troponin special where we delve deeper into high sensitivity troponins (hs-Tn) and their significance in emergency medicine. Today, we'll explore the nuances of hs-Tn assays and how they can enhance our work in the emergency department (ED).
Introduction to High Sensitivity Troponins
High sensitivity troponins (hs-Tn) have transformed how we detect and manage myocardial infarctions (MI) in emergency settings. Unlike traditional assays, hs-Tn tests detect much lower concentrations of troponin, a protein released during myocardial injury, allowing for earlier and more accurate detection of cardiac events.
Analytical Sensitivity vs. Diagnostic Sensitivity
Understanding the difference between analytical and diagnostic sensitivity is crucial. Analytical sensitivity refers to the assay's ability to detect low concentrations of troponin, whereas diagnostic sensitivity relates to the test's performance in diagnosing acute myocardial infarctions (AMI).
Key Points on Analytical Sensitivity:
- Detection Threshold: High sensitivity troponin assays can detect troponin in over 50% of healthy individuals.
- Precision: These assays have a coefficient of variation (CV) of less than 10% at the diagnostic threshold, ensuring consistent results.
Diagnostic Sensitivity:
- Improved Detection: Studies show hs-Tn assays have a higher diagnostic sensitivity (90-92%) compared to older assays (80-85%).
- Early Rule-Outs: This makes hs-Tn particularly valuable for ruling out AMI in patients presenting with chest pain in the ED.
High Sensitivity Troponin Assays: A Closer Look
To illustrate, let's focus on the Roche troponin T high sensitivity assay:
- 99th Percentile Cutoff: 14 nanograms per liter.
- Detection Range: Can detect levels as low as 3 nanograms per liter.
- Higher Readings: It's common for hs-Tn assays to give higher readings than older assays for the same sample, which affects the diagnostic threshold.
The Balance Between Sensitivity and Specificity
While hs-Tn assays improve sensitivity, they may reduce specificity:
- More Positives: Lowering the diagnostic threshold results in more positive results, increasing diagnostic sensitivity but reducing specificity.
- Predictive Value: For example, a positive hs-Tn T result at patient arrival has a specificity around 70% and a positive predictive value of 50%.
Using High Sensitivity Troponins in the Emergency Department
Early Rule-Out Protocols: The most significant advantage of hs-Tn assays is their potential to expedite the rule-out process:
- Zero and Three-Hour Protocols: Studies suggest that hs-Tn assays can effectively rule out AMI with samples taken at 0 and 3 hours after arrival, instead of the traditional 6-hour wait.
- Efficiency: This protocol can significantly speed up patient throughput in the ED, reducing congestion and wait times.
Understanding Deltas: Delta refers to the change in troponin levels between tests:
- Absolute vs. Relative Deltas: Absolute changes (e.g., an increase of 10 nanograms per liter) are often more reliable than relative percentage changes.
- Clinical Context: It's crucial to interpret deltas in the context of the patient's overall clinical picture.
Practical Considerations for Emergency Physicians
Incidental Troponin Elevations: With increased testing at the front door, incidental findings are inevitable:
- Low Pre-Test Probability: In patients with a low pre-test probability of AMI (e.g., mechanical falls), a positive hs-Tn result often does not indicate AMI.
- Clinical Judgment: Consider repeating the test and evaluating the patient's history and clinical presentation before making a decision.
Patients with Comorbidities: Troponin levels can be elevated in patients with various comorbidities:
- Age and Chronic Conditions: Older patients and those with conditions like LV dysfunction may have higher baseline troponin levels.
- Reference Ranges: Use broader reference ranges for patients with comorbidities, as suggested by studies from Paul Collins and colleagues.
Future Directions and Guidelines
Ongoing Research: Research and guidelines on hs-Tn usage are continually evolving:
- NICE Guidelines: Recommendations on using hs-Tn in clinical practice are expected to be published, providing clearer protocols for emergency physicians.
- Early Adoption: As new evidence emerges, early adopters must balance innovation with patient safety.
Point-of-Care Testing: While hs-Tn assays currently require large analyzers, point-of-care testing remains a goal:
- Future Developments: Advances in technology may eventually make hs-Tn testing available at the bedside, further streamlining ED workflows.
Conclusion
High sensitivity troponins represent a significant advancement in the early detection and management of myocardial infarctions in the emergency department. By understanding the nuances of analytical and diagnostic sensitivity, utilizing early rule-out protocols, and interpreting results within the clinical context, emergency physicians can leverage these assays to improve patient care. As always, ongoing research and adherence to evolving guidelines will be essential in optimizing the use of hs-Tn in clinical practice.
We hope this podcast helps you better understand the complexities and advantages of high sensitivity troponins. For more insights and updates, stay tuned to the St. Emlyn's blog and feel free to reach out with your questions and experiences. Together, we can continue to advance emergency medicine for the benefit of our patients.

Wednesday Aug 06, 2014
Ep 14 - Exeter CEM conference with Adam Reuben
Wednesday Aug 06, 2014
Wednesday Aug 06, 2014
College of Emergency Medicine Conference 2024: Everything You Need to Know
Welcome to the St. Emlyne's blog, where we provide the latest updates and insights into the world of emergency medicine. Today, we're diving into the much-anticipated College of Emergency Medicine (CEM) Conference, set to take place in Exeter from September 9th to 11th. This conference is not only a hub for academic learning but also a celebration of the progress and future of emergency medicine.
Why Exeter?
Exeter, nestled in the scenic Southwest of England, offers an exciting venue for this year’s CEM Conference. The University of Exeter provides a fresh and dynamic backdrop, allowing attendees to experience a new environment. The choice of Exeter also aims to highlight the region's significant contributions to medical research and practice. Plus, the location promises better weather compared to other parts of the UK, making it a pleasant destination.
Key Highlights and Speakers
The conference is packed with sessions designed to engage and educate emergency medicine professionals. Here are some highlights to look forward to:
Inspirational Talks and Keynote Speakers
- Ann Marie Kelly from Australia will share her expertise on arterial and venous blood gases, offering critical insights for daily medical practice.
- James Robson, doctor to the Scottish rugby team and the British and Irish Lions, will discuss the pressures and challenges of pitchside medicine and his experiences over the past 15 to 20 years.
- Cliff Reed, a renowned figure in emergency medicine, will inspire attendees with his motivational presentations.
- Cliff Mann, the current college president, will discuss clinical topics, reflecting his deep involvement in frontline emergency medicine.
Engaging Sessions
The conference features a variety of sessions tailored to different interests within emergency medicine:
- Dragon's Den: Watch as grant applicants pitch their projects to a panel of emergency medicine experts, competing for a share of £1000 to fund their innovative ideas.
- Stroke Management: Jason Kendall will provide an in-depth look at stroke management and the latest research in this critical area.
Social and Networking Events
Balancing work with social activities is a key theme of the conference. Highlights include:
- Gala Dinner at Exeter Castle: An opportunity to unwind and network in a historic setting.
- Explore Devon Activities: From surfing at Bantham to paddleboarding on the River Exe, there are plenty of outdoor activities. Attendees can also enjoy kayaking, mountain biking, or exploring local museums.
Academic Excellence
The conference boasts a robust academic programme with four tracks running simultaneously on some days, ensuring there's something for everyone, whether you're a trainee, an established consultant, or involved in cutting-edge emergency medicine research.
Core Emergency Medicine Topics
Sessions focus on essential topics in emergency medicine, aiming to reconnect professionals with the fundamentals that make this field vital and rewarding. The goal is to address rising attendances and increasing pressures in emergency departments by reinforcing core knowledge and practices.
Cutting-Edge Research
Attendees will engage with the latest research and innovations in emergency medicine. The programme is designed to be both educational and academically stimulating, attracting participants with its high-quality content.
Why Attend?
The CEM Conference in Exeter offers numerous benefits:
- Professional Development: Enhance your knowledge and skills through sessions led by top experts in the field.
- Networking: Connect with colleagues from across the country and beyond, sharing experiences and best practices.
- Inspiration: Gain new perspectives and motivation from leading figures in emergency medicine.
- Fun and Relaxation: Enjoy the social events and explore the beautiful surroundings of Exeter and Devon.
Practical Information
Booking and Availability
If you haven't booked your place yet, it’s not too late! There are still a few spots available, but they are filling up fast. Visit the college website to secure your place and register for the explore Devon activities, which are also in high demand.
Staying Updated
For those who can’t attend in person, the conference will share video excerpts of key sessions. Follow the #CEMEXETER2014 hashtag on Twitter and check out the college's YouTube channel for updates and highlights.
Conclusion
The CEM Conference in Exeter is shaping up to be an unmissable event for anyone in the field of emergency medicine. With its combination of high-quality academic content, inspirational speakers, and engaging social activities, it promises to be both educational and enjoyable. Whether you're attending for the learning opportunities, the chance to network, or simply to enjoy the vibrant atmosphere, this conference has something to offer everyone.
Don't miss out on this fantastic opportunity to advance your career and connect with the emergency medicine community. Book your place today and join us in Exeter for an unforgettable experience!
Sunday Jul 27, 2014
Ep - 11 Understanding Troponin Part 1
Sunday Jul 27, 2014
Sunday Jul 27, 2014
The Ultimate Guide to Understanding Troponins in Emergency Medicine
Welcome to the St. Emlyn's podcast! In this episode, we're exploring the fascinating world of troponins, vital biomarkers essential for diagnosing myocardial injury. Whether you're a seasoned clinician or a medical student, understanding troponins is crucial for effective patient care. We'll cover everything from the basics to advanced concepts, ensuring you have a comprehensive grasp of this critical topic.
What are Troponins?
Troponins are proteins found in muscle tissue, playing a key role in muscle contraction. Often misunderstood as cardiac enzymes, troponins are actually proteins involved in the contractile apparatus within muscle cells. They exist in three forms: Troponin I, Troponin T, and Troponin C, which work together within muscle fibers to regulate muscle contractions.
Why are Troponins Important in Cardiology?
Troponins are crucial biomarkers for diagnosing myocardial injury. When heart muscle is damaged, troponins are released into the bloodstream. This release can occur due to various conditions, including myocardial infarction (heart attack) and other forms of stress on the heart. Measuring troponin levels in the blood helps clinicians determine the extent of myocardial injury and make informed decisions about patient care.
The Difference Between Cardiac and Skeletal Troponins
Troponins are present in both skeletal and cardiac muscle. However, cardiac-specific isoforms of Troponin I and Troponin T can be detected through blood tests, allowing clinicians to specifically identify myocardial damage. This specificity is a significant advancement over previous markers like CK, LDH, and ALT, which were not cardiac-specific and took longer to rise in the bloodstream.
When are Troponins Released into the Blood?
Troponins are released into the bloodstream when there is myocardial injury. This injury can result from various causes, such as acute myocardial infarction, physical stress, or other conditions that strain the heart. Understanding that troponins indicate myocardial injury rather than just myocardial infarction is crucial for accurate diagnosis and treatment.
The Kinetics of Troponin Release
Following myocardial injury, troponin levels typically peak in the blood within 12 to 24 hours. The time it takes for troponin levels to fall depends on several factors, including the severity of the injury, the patient's renal function, and whether there is ongoing troponin release into the blood. For example, patients with significant myocardial infarction might take weeks to clear troponins from their bloodstream, while those with smaller injuries might clear them within a day.
Troponins and Renal Failure
A common question is whether troponin tests are useful in patients with renal failure. The answer is a resounding yes. Although patients with renal failure may have elevated baseline troponin levels due to reduced clearance, troponin testing remains a valuable diagnostic tool. It's essential to interpret these levels in the context of the patient's renal function and look for trends in troponin levels through serial testing.
Understanding Troponin Assays
Troponin tests are immunoassays, which means they use antibodies to target specific parts of the troponin molecule. These antibodies are attached to a signal that emits light, allowing for the quantification of troponin levels in the blood. While lab-based assays are highly accurate, point-of-care testing devices are also available, though they may not be as sensitive or precise as lab tests.
The Role of Point-of-Care Testing
Point-of-care testing devices, such as handheld analyzers, offer quick results and can be used at the bedside. However, they may not match the sensitivity and precision of lab-based assays. Some portable devices provide qualitative results, similar to a home pregnancy test, while others offer quantitative measurements. Clinicians should be aware of these differences and use point-of-care devices appropriately.
Analytical vs. Diagnostic Sensitivity
When discussing troponin assays, it's crucial to differentiate between analytical sensitivity and diagnostic sensitivity. Analytical sensitivity refers to the assay's ability to detect low concentrations of troponin reliably. In contrast, diagnostic sensitivity pertains to the assay's ability to correctly identify patients with the condition being tested for, such as acute myocardial infarction. High-sensitivity troponin assays have improved both analytical and diagnostic sensitivity, enabling earlier and more accurate diagnosis.
Timing of Troponin Testing
In the UK, troponin testing typically starts from the time of symptom onset. This approach differs from other countries where testing begins upon the patient's arrival in the emergency department. The timing of troponin testing is crucial, as early testing can lack sensitivity. Serial sampling over several hours helps ensure accurate diagnosis, with a common practice being to test initially and then again at intervals such as six, ten, or twelve hours after symptom onset.
Interpreting Troponin Levels in Clinical Practice
Interpreting troponin levels requires considering the clinical context and pre-test probability. A positive troponin test in a patient with low pre-test probability of myocardial infarction may not indicate a true positive. Conversely, a negative test in a high-risk patient does not entirely rule out disease, especially if there is potential for a late troponin rise. Clinicians must integrate troponin results with other diagnostic information to make informed decisions.
Troponins in Renal Failure
Patients with renal failure often have elevated baseline troponin levels due to impaired clearance. However, troponin testing remains valuable for diagnosing myocardial injury in these patients. It's essential to understand the baseline level for each patient and focus on changes in troponin levels over time, rather than a single measurement. Serial sampling helps differentiate chronic elevation from acute myocardial injury.
Diagnosing Unstable Angina
It's important to recognize that unstable angina can occur without elevated troponin levels. These patients may not show a rise and fall in troponin but still have significant coronary artery disease that requires attention. Clinical judgment, along with other diagnostic tools like ECG and patient history, is vital in diagnosing and managing unstable angina.
Key Takeaways for Clinicians
- Troponins are proteins involved in muscle contraction and are critical biomarkers for diagnosing myocardial injury.
- Cardiac-specific isoforms of Troponin I and Troponin T are used to detect myocardial damage through blood tests.
- Troponins are released into the blood following myocardial injury, not just myocardial infarction.
- The timing of troponin testing is crucial, with serial sampling providing more accurate results.
- Point-of-care testing devices offer quick results but may lack the sensitivity and precision of lab-based assays.
- Interpreting troponin levels requires considering the clinical context and pre-test probability.
- Troponin testing is valuable in patients with renal failure, focusing on changes in levels over time.
- Unstable angina can occur without elevated troponin levels, requiring careful clinical evaluation.
Conclusion
Understanding troponins and their role in diagnosing myocardial injury is essential for clinicians. From the basics of what troponins are to the nuances of interpreting test results, this knowledge is crucial for providing the best care to patients with suspected cardiac conditions. Stay tuned for our next episode, where we'll delve deeper into high-sensitivity troponin assays and their impact on emergency medicine.
For any questions or further discussion, feel free to comment on the blog post or email us. We're here to help and look forward to continuing this conversation. Until next time, take care and keep learning!
This blog post is brought to you by the team at St. Emlyn's, dedicated to providing high-quality education and resources for emergency medicine professionals.

Monday Jul 21, 2014
Ep 10 - Intro to EM: Staying safe in your first job
Monday Jul 21, 2014
Monday Jul 21, 2014
Starting Your Career in Emergency Medicine: Key Insights from St. Emlyn’s
Welcome to the world of emergency medicine! At St. Emlyn’s, we understand the challenges and excitement that come with starting your career in this fast-paced field. Whether you’re a new doctor stepping into the emergency department (ED) for the first time or a medical student gearing up for your rotation, we’ve got you covered. This post delves into the nuances of emergency medicine, sharing valuable insights from seasoned professionals, Iain Beardsell and Simon Carley, to help you navigate your journey effectively.
Understanding the Unique Nature of Emergency Medicine
Emergency medicine is distinct from other medical disciplines. Unlike the traditional approach taught in medical school, which involves extensive histories and comprehensive examinations, emergency medicine requires quick, focused thinking and decisive action. The goal is to identify and address life-threatening conditions promptly.
Time-Pressured Environment
In the ED, time is of the essence. Patients arrive needing immediate care, and as an emergency physician, you won’t have the luxury of lengthy deliberations. Your patients want answers quickly, and this urgency shapes the way you practice. You’ll learn to focus on the presenting problem and drill down into the most critical aspects of their condition.
Different Thinking Model
The thinking model in emergency medicine is primarily hyperthetico-deductive reasoning. This means you’ll form hypotheses based on initial information and then test these hypotheses through targeted questions and examinations. For instance, if a 55-year-old man presents with central crushing chest pain radiating down his left arm, your first thought should be an acute myocardial infarction (AMI).
Prioritizing Life-Threatening Conditions
One of the fundamental differences in emergency medicine is the approach to diagnosing and treating conditions. Instead of trying to confirm what a patient has, you’ll focus on ruling out what they don’t have, especially the most life-threatening possibilities. For example, with chest pain, you’ll consider AMI, pulmonary embolism (PE), and aortic dissection as top priorities.
The 10% Rule
Interestingly, about 10% of patients presenting with symptoms like chest pain or headache have significant pathology. Your job is to identify this 10% while efficiently managing the remaining 90%. This approach ensures that you don’t miss critical diagnoses while not overburdening yourself with unnecessary details.
Practical Steps for Your First Shift
As you prepare for your first shift in the ED, here are some practical steps and philosophies to keep in mind:
Resuscitation First
Your primary goal is to identify if a patient needs resuscitation. Are they critically unwell? Do they require urgent interventions to save their life? This is your top priority.
Pain Management
After ensuring resuscitation, your next focus should be pain management. A pain-free emergency department is a goal to strive for. Administer analgesia as needed to ensure patient comfort, even before completing a full history or examination.
Rule Out Life-Threatening Conditions
When a patient presents with a complaint, think about the worst-case scenarios related to their symptoms and aim to rule these out. For example, with chest pain, consider whether the patient might have an AMI, PE, or aortic dissection.
Focused History and Examination
Conduct a focused history and examination to gather information pertinent to the presenting complaint. Avoid getting bogged down with irrelevant past medical history unless it directly impacts the current situation.
Implementing the Four Big Hitters
Simon and Iain emphasize the importance of considering four key interventions for every patient:
- Oxygen: Determine if the patient needs oxygen or airway support.
- Analgesia: Ensure adequate pain relief is provided.
- Fluids: Assess if the patient would benefit from intravenous fluids.
- Antibiotics: Consider if antibiotics are necessary for their condition.
Learning and Growing in the ED
The ED is a dynamic learning environment. Here’s how you can maximize your growth and effectiveness:
Ask Questions
Don’t hesitate to ask questions. No question is too silly. Engaging with senior colleagues and seeking their advice will enhance your learning and patient care skills.
Continuous Learning
Emergency medicine is a field where continuous learning is crucial. Keep up with the latest practices, guidelines, and innovations. Attend workshops, conferences, and training sessions to stay updated.
Collaborative Approach
Remember that emergency medicine is a team effort. Collaborate with nurses, paramedics, and other healthcare professionals. Effective communication and teamwork are essential for providing the best patient care.
Reflect and Improve
After each shift, take time to reflect on your experiences. Identify what went well and areas for improvement. This self-assessment will help you grow as a clinician and enhance your skills over time.
The Importance of Confidence and Competence
Confidence in your abilities is vital, but it must be balanced with competence. Strive to be competent in your practice, and your confidence will naturally follow. Be aware of the balance between these two aspects to avoid the pitfalls of overconfidence.
Unconscious Incompetence
One of the dangers in any medical field is unconscious incompetence—being unaware of what you don’t know. Stay humble, keep learning, and seek feedback from peers and seniors to continuously improve your competence.
Embracing the ED Culture
The culture in the ED is unique. It’s a place where decisive actions and quick thinking are valued. Embrace this culture and the opportunities it presents for hands-on learning and making a real difference in patients’ lives.
A Little Less Conversation, A Little More Action
In the ED, the Elvis philosophy—“a little less conversation, a little more action”—applies. Focus on doing what’s necessary for the patient rather than getting caught up in lengthy discussions. This action-oriented approach is crucial for effective emergency care.
Conclusion: Your Journey Ahead
Starting your career in emergency medicine is both exciting and challenging. At St. Emlyn’s, we believe in providing you with the tools, knowledge, and support you need to succeed. Remember the key principles: prioritize life-threatening conditions, focus on critical interventions, continuously learn and ask questions, and embrace the dynamic culture of the ED.
We love our jobs and hope that you, too, will find the same passion and fulfillment in your career. Good luck, enjoy the journey, and know that we’ll be with you every step of the way through this podcast and our wider St. Emlyn’s community.
Welcome to the world of emergency medicine. Let’s make a difference together!
